Abstract
Aims
The aim of this study was to assess the effectiveness and safety of vaginal native tissue repair (VNTR) as a surgical treatment for severe pelvic organ prolapse (POP) and, second, to evaluate the impact on the quality-of-life (QoL) and sexual function.
Methods
Women with symptomatic POP (≥III stage according to POP Quantification System) with or without stress urinary incontinence (SUI) underwent VNTR. The clinical stage, 3-day voiding diary, and urodynamic testing were evaluated in the preoperative and postoperative times, respectively. The International Consultation on Incontinence Questionnaire–Urinary Incontinence Questionnaire Short Form (ICIQ–UI SF), the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire short form (PISQ-12), and the prolapse quality-of-life questionnaire (P-QoL) were administered.
Results
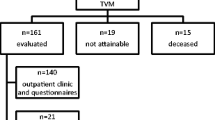
One hundred forty-six patients were recruited. The median follow-up was 48 months (36–63). Fifty-two women (36%) had a previous hysterectomy, and 16 (11%) had a previous prolapse/continence surgery. Preoperatively, 135 (92.5%), 109 (74.7%), and 98 (67.1%) patients had anterior, central, and posterior descent ≥III stage, respectively. Thirty-two patients (22%) had concomitant diagnosis of SUI. Median operative time was 85 min (37–154), and median postoperative hospital stay was 2 days (2–4). No intraoperative severe complications occurred. At the long-term follow-up, the subjective cure rate for prolapse was 97.3% and the objective cure rate was 91.1%. A significant improvement of ICIQ-UI SF, the P-QoL, and the PISQ-12 was recorded at the follow-up (p < 0.001).
Conclusion
VNTR is effective, safe, and durable and improves POP-related symptoms and sexual function.
Similar content being viewed by others
References
Nygaard I, Barber MD, Burgio KL et al (2008) Prevalence of symptomatic pelvic floor disorders in US women. JAMA 300:1311–1316
Wu JM, Hundley AF, Fulton RG et al (2009) Forecasting the prevalence of pelvic floor disorders in U.S. Women: 2010 to 2050. Obstet Gynecol 114:1278–1283
Vergeldt TFM, Weemhoff M, Inthout J et al (2015) Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J 26:1559–1573
FDA Safety Communication (2011) Urogynecologic surgical mesh: update on the safety and effectiveness of transvaginal placement for pelvic organ prolapse. Issued 13 July 2011
Funk JM, Visco AG, Weidner AC et al (2013) Long-term outcomes of vaginal mesh versus native tissue repair for anterior vaginal wall prolapse. Int Urogynecol J 24:1279–1285
Wei JT, De Lancey JO (2004) Functional anatomy of the pelvic floor and lower urinary tract. Clin Obstet Gynecol 47:3–17
Farthmann J, Watermann D, Erbes T et al (2015) Functional outcome after pelvic floor reconstructive surgery with or without concomitant hysterectomy. Arch Gynecol Obstet 291:573–577
Maher C, Feiner B, Baessler K et al (2013) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 30(4):CD004014
Farthmann J, Mengel M, Henne B et al (2016) Improvement of pelvic floor-related quality of life and sexual function after vaginal mesh implantation for cystocele: primary endpoint of a prospective multicentre trial. Arch Gynecol Obstet 294:115–121
Espuna-Pons M, Dilla T, Castro D (2007) Analysis of the value of the ICIQ-UI SF questionnaire and stress test in the differential diagnosis of the type of urinary incontinence. Neurourol Urodyn 26:836–841
Visco AG, Wei JT, McClure LA et al (2003) Effects of examination technique modifications on pelvic organ prolapse quantification (POP-Q) results. Int Urogynecol J Pelvic Floor Dysfunct 14:136–140
Rogers GR, Coates KW, Kammerer-Doak D et al (2001) A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct 12:361–365
Digesu GA, Santamato S, Khullar V et al (2003) Validation of an Italian version of the prolapse quality of life questionnaire. Eur J Obstet Gynecol Reprod Biol 106:184–192
Shull BL, Bachofen C, Coates KW et al (2000) A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol 183:1365–1374
Weber AM, Walters MD, Piedmonte MR, Ballard LA (2001) Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol 185:1299–1306
De Leval J (2003) Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol 44:724–730
Samour H, Amgad Abougamra A, Sabaa HAM (2011) Minimally invasive cystocele repair technique using a polypropylene mesh introduced with the transobturator route. Arch Gynecol Obstet 291:79–84
Maher C, Feiner B, Baessler K et al (2016) Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse (Review). Cochrane Database Syst Rev Issue 2 Art. No.: CD012079
Altman D, Vayrynen T, Engh ME et al (2011) Anterior colporrhaphy versus transvaginal mesh for pelvic-organ. N Engl J Med 364:1826–1836
Siff LN, Barber MD (2016) Native tissue prolapse repairs: comparative effectiveness trials. Obstet Gynecol Clin North Am 43:69–81
Marschke J, Hengst L, Schwertner-Tiepelmann N et al (2015) Transvaginal single-incision mesh reconstruction for recurrent or advanced anterior vaginal wall prolapse. Arch Gynecol Obstet 291:1081–1087
Spelzini F, Frigerio M, Manodoro S et al (2016) Modified McCall culdoplasty versus Shull suspension in pelvicprolapse primary repair: a retrospective study. Int Urogynecol J 016-3016-6
Wein AJ (2015) Re: Comparison of 2 transvaginal surgical approaches and perioperative behavioral therapy for apical vaginal prolapse: the OPTIMAL randomized trial. J Urol 193:943–944
Diwadkar GB, Barber MD, Feiner B et al (2009) Complication and reoperation rates after apical vaginal prolapse surgical repair: a systematic review. Obstet Gynecol 113:367–373
Paraiso MF, Barber MD, Muir TW et al (2006) Rectocele repair: a randomized trial of three surgical techniques including graft augmentation. Am J Obstet Gynecol 195:1762–1771
Withagen MI, Milani AL, De Leeuw JW et al (2012) Development of de novo prolapse in untreated vaginal compartments after prolapse repair with and without mesh: a secondary analysis of a randomised controlled trial. BJOG Int J Obstet Gynaecol 10:1471–1528
Mothes AR, Radosa MP, Altendorf-Hofmann A et al (2016) Risk index for pelvic organ prolapse based on established individual risk factors. Arch Gynecol Obstet 293:617–624
Zullo MA, Ruggiero A, Plotti F et al (2008) Anterior colporrhaphy plus inside-out tension-free vaginal tape for associated stress urinary incontinence and cystocele. J Minim Invasive Gynaecol 15:446–451
Ling C, Chang Y, Lin Y, Chang S (2013) Significance of bladder trabeculation in postmenopausal women with severe pelvic organ prolapse: clinical and urodynamic assessments. Menopause 20:813–817
Jha S, Gray T (2015) A systematic review and meta-analysis of the impact of native tissue repair for pelvic organ prolapse on sexual function. Int Urogynecol J 26:321–327
Mothes AR, Mothes HK, Radosa MP et al (2015) Systematic assessment of surgical complications in 438 cases of vaginal native tissue repair for pelvic organ prolapse adopting Clavien–Dindo classification. Arch Gynecol Obstet 291:1297–1301
Vitale SG, Caruso S, Rapisarda AMC et al (2016) Biocompatible porcine dermis graft to treat severe cystocele: impact on quality of life and sexuality. Arch Gynecol Obstet 293:125–131
Katsara A, Wight E, Heinzelmann-Schwarz V et al (2016) Long-term quality of life, satisfaction, pelvic floor symptoms and regret after colpocleisis. Arch Gynecol Obstet 294:999–1003
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Michele Carlo Schiavi declares that he has no conflict of interest. Author Giorgia Perniola declares that she has no conflict of interest. Author Violante Di Donato declares that he has no conflict of interest. Author Virginia Sibilla Visentin declares that she has no conflict of interest. Author Flaminia Vena declares that she has no conflict of interest. Author Anna Di Pinto declares that she has no conflict of interest. Author Mario Angelo Zullo declares that he has no conflict of interest. Author Marco Monti declares that he has no conflict of interest. Author Pierluigi Benedetti Panici declares that he has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Authors’ contributions
All the authors contributed equally to this study. Michele Carlo Schiavi: Project development, Data Collection, Manuscript writing. Giorgia Perniola: Project development, Data Collection, Manuscript writing. Violante Di Donato: Project development, Data Collection, Manuscript writing. Marco Monti: Project development, Data Collection, Manuscript writing. Virginia Sibilla Visentin: Project development, Data Collection, Manuscript writing. Flaminia Vena: Project development, Data Collection, Manuscript writing. Anna Di Pinto: Project development, Data Collection, Manuscript writing. Marzio Angelo Zullo: Project development, Data Collection, Manuscript writing. Pierluigi Benedetti Panici: Project development, Data Collection, Manuscript writing.
Rights and permissions
About this article
Cite this article
Schiavi, M.C., Perniola, G., Di Donato, V. et al. Severe pelvic organ prolapse treated by vaginal native tissue repair: long-term analysis of outcomes in 146 patients. Arch Gynecol Obstet 295, 917–922 (2017). https://doi.org/10.1007/s00404-017-4307-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4307-y