Abstract
Objective
To compare the efficacy of preinduction outpatient use of a single dose of 25 μg vaginal misoprostol between 381/2 and 40 weeks with that of placebo, to decrease the interval from intervention to delivery after stretch and sweep in low-risk gravid women with Bishop’s score <4.
Method
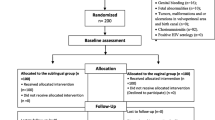
Sixty three women received 25 μg vaginal misoprostol and 63 women received placebo after stretch and sweep.
Results
The duration from intervention to delivery was 3.35 (1.12–9.46) days in the misoprostol group and 5.42 (2.39–10.11) days in the placebo group which was statistically significant (p = 0.029). Spontaneous labor was seen in 39 women (61.9 %) in the misoprostol group and 35 women (55.6 %) in the placebo group (p = 0.531). Eight women in the misoprostol group and 18 in the placebo group had Lower Segment Caesarean Section (LSCS) and this difference was also statistically significant (p = 0.027). There were no major maternal and neonatal complications in both groups.
Conclusion
Preinduction use of 25 μg vaginal misoprostol after stretch and sweep in the outpatient setting decreased the intervention to delivery interval when compared to placebo.

Similar content being viewed by others
References
Olesen AW, Westergaard JG, Olsen J (2003) Perinatal and maternal complications related to postterm delivery: a national register-based study, 1978–1993. Am J Obstet Gynecol 189(1):222–227
Joseph KS (2011) The natural history of pregnancy: diseases of early and late gestation. BJOG Int J Obstet Gynaecol 118(13):1617–1629
World Health Organization (2011) WHO recommendations for induction of labor. World Health Organization, Geneva, (WHO Guidelines Approved by the Guidelines Review Committee). Available from http://www.ncbi.nlm.nih.gov/books/NBK131963/. Accessed 25 Aug 2016
Mandruzzato G, Alfirevic Z, Chervenak F, Gruenebaum A, Heimstad R, Heinonen S et al (2010) Guidelines for the management of postterm pregnancy. J Perinat Med 38:111–119
Morris JM, Thompson K, Smithey J, Gaffney G, Cooke I, Chamberlain P, Hope P, Altman D, MacKenzie IZ (2003) The usefulness of ultrasound assessment of amniotic fluid in predicting adverse outcome in prolonged pregnancy: a prospective blinded observational study. BJOG Int J Obstet Gynaecol 110(11):989–994
Ugwu EO, Obi SN, Iferikigwe ES, Dim CC, Ezugwu FO (2014) Membrane stripping to prevent post-term pregnancy in Enugu, Nigeria: a randomized controlled trial. Arch Gynecol Obstet 289(1):29–34
Boulvain M, Stan CM, Irion O (2005) Membrane sweeping for induction of labour. Cochrane Database Syst Rev (1):CD000451. doi:10.1002/14651858.CD000451.pub2.
Goldberg AB, Greenberg MB, Darney PD (2001) Misoprostol and pregnancy. N Engl J Med 344(1):38–47
National Institute for Health and Care Excellence (2015) Induction of labor. https://www.nice.org.uk/guidance/cg70/. Published July 2008. Accessed 21 Jan 2015
ACOG Committee on Practice Bulletins–Obstetrics (2009) ACOG Practice Bulletin No. 107: Induction of labor. Obstet Gynecol 114:386
Hofmeyr GJ, Gülmezoglu AM, Pileggi C (2010) Vaginal misoprostol for cervical ripening and induction of labor. Cochrane Database Syst Rev 10:CD000941
McMaster K, Sanchez-Ramos L, Kaunitz AM (2015) Balancing the efficacy and safety of misoprostol: a meta-analysis comparing 25 versus 50 micrograms of intravaginal misoprostol for the induction of labour. BJOG Int J Obstet Gynaecol 122(4):468–476
Calder AA, Loughney AD, Weir CJ, Barber JW (2008) Induction of labour in nulliparous and multiparous women: a UK, multicentre, open-label study of intravaginal misoprostol in comparison with dinoprostone. BJOG Int J Obstet Gynaecol 115(10):1279–1288
Oboro VO, Tabowei TO (2005) Outpatient misoprostol cervical ripening without subsequent induction of labor to prevent post-term pregnancy. Acta Obstet Gynecol Scand 84:628–631. doi:10.1111/j.0001-6349.2005.00655.x
Teixeira C, Lunet N, Rodrigues T, Barros H (2012) The Bishop Score as a determinant of labour induction success: a systematic review and meta-analysis. Arch gynecol obstet 286(3):739–753
Stitely ML, Browning J, Fowler M, Gendron RT, Gherman RB (2000) Outpatient cervical ripening with intravaginal misoprostol. Obstet Gynecol 96(5, Part 1):684–688
Javadekar D, Rokade A, Alchemy V (2013) Can term gestation be induced by misoprostol on OPD basis? J Evol Med Dent Sci 1(2):3929–3936
Adeniji AO, Akinola E (2013) A comparison of orally administered misoprostol and membrane sweeping for labour induction in uncomplicated singleton post-term pregnancies. S Afr J Obstet Gynaecol 19(1):4–7
Incerpi MH, Fassett MJ, Kjos SL, Tran SH, Wing DA (2001) Vaginally administered misoprostol for outpatient cervical ripening in pregnancies complicated by diabetes mellitus. Am J Obstet Gynecol 185(4):916–919
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Rights and permissions
About this article
Cite this article
PonMalar, J., Benjamin, S.J., Abraham, A. et al. Randomized double-blind placebo controlled study of preinduction cervical priming with 25 µg of misoprostol in the outpatient setting to prevent formal induction of labour. Arch Gynecol Obstet 295, 33–38 (2017). https://doi.org/10.1007/s00404-016-4173-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4173-z