Abstract
Purpose
The aim of this study is to identify the rate of incisional hernias and associated risk factors following a vertical midline laparotomy on a gynecologic oncology service.
Methods
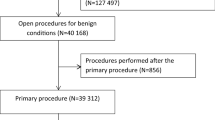
This is a retrospective cohort study of patients that underwent a laparotomy through a vertical midline abdominal incision between September 1998 and November 2012. Hernias and various factors were identified including demographics, disease comorbidities, intraoperative variables, and suture technique. Assessment of association with hernia formation was performed using Cox regression and log-rank test.
Results
Two hundred and fifty-two patients with follow-up of at least 30 days were identified. Mean age was 59 years (range 21–88 years) and mean BMI was 35.9 kg/m2 (range 17.2–84.4 kg/m2). Sixteen (6.3 %) developed incisional hernias with a median follow-up of 1.7 years (range 1 month to 13 years). The estimate of the 5-year probability of being hernia-free is 86 % (95 % CI 76.5–91.9). Average age of patients who developed a hernia was 66.2 years while average age of those without hernia was 58 years (p < 0.05). There was a significant association of hypertension with incisional hernia occurrence (p = 0.0035, log-rank test). Cancer was present in 100 % of patients that developed hernias and 73 % (172/236) of those that were hernia-free (p = 0.0041, log-rank test). By univariate analysis the risk of developing an incisional hernia was higher, if the abdominal fascia was closed with loop sutures (HR 4.6, 95 % CI 1.49–13.94; p = 0.008). By multivariable analysis incisions closed with loop suture had more than a fivefold increased risk of developing a hernia (HR 5.2, 95 % CI 1.65–16.39; p = 0.005). Presence of both hypertension and utilization of loop sutures had the highest risk of incisional hernia development (HR 7.1, 95 % CI 2.28–22.4; p = 0.001).
Conclusion
Wound complications including incisional hernias contribute to morbidity in gynecologic oncology patients. Older age, hypertension, utilization of loop sutures, and cancer were found to be associated with hernia formation after laparotomy through a vertical midline abdominal incision. The use of loop sutures to close the abdominal fascia should be investigated further.

Similar content being viewed by others
References
O’Dwyer PJ, Courtney CA (2003) Factors involved in abdominal wall closure and subsequent incisional hernia. Surg J R Coll Surg Edinb Irel 1:17–22
Burger JW, Luikendijk RW, Hop WC, Halm JS, Verdaasdonk GG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583
Hodgson NC, Malthaner RA, Østbye T (2000) The search for an ideal method of abdominal fascial closure: a meta-analysis. Ann Surg 231:436–442
Israellsson LA, Millbourn D (2013) Prevention of incisional hernias. How to close a midline incision. Surg Clin N Am 93:1027–1040
Poole GV (1985) Mechanical factors in abdominal wound closure: the prevention of fascial dehiscence. Surgery 97:631–640
Höer J, Lawong G, Klinge U, Schumpelick V (2002) Factors influencing the development of incisional hernia: a retrospective study of 2,983 laparotomy patients over a period of 10 years. Chirurg 73:474–480
Goodenough CJ, Ko TC, Kao LS et al (2015) Development and validation of a risk stratification score for ventral incisional hernia after abdominal surgery: hernia expectation rates in intra-abdominal surgery (the hernia project). J Am Coll Surg 220:405–415
Spencer RJ, Hayes KD, Rose S et al (2015) Risk factors for early-occurring and late-occurring incisional hernias after primary laparotomy for ovarian cancer. Obstet Gynecol 125:407–413
Israelsson LA, Jonsson T (1996) Incisional hernia after midline laparotomy: a prospective study. Eur J Surg 162:125–129
Israelsson LA, Jinsson T (1993) Suture length to wound length ratio and healing of midline laparotomy incisions. Br J Surg 80:1284–1286
Rettenmaier MA, Abaid LN, Brown JV, Micha JP, Goldstein BH (2009) Chemotherapy and patient co-morbidity in ventral site hernia development. Gynecol Oncol 20:246–250
Franchi M, Ghezzi F, Buttarelli M, Tateo S, Balestreri D, Bolis P (2001) Incisional hernia in gynecologic oncology patients: 10-year study. Obstet Gynecol 97:696–700
Long KC, Levinson KL, Diaz JP, Gardner GJ, Chi DS, Barakat RR, Leitao MM Jr (2011) Ventral hernia following primary laparotomy for ovarian, fallopian tube, and primary peritoneal cancers. Gynecol Oncol 120:33–37
Milbourn D, Cengiz Y, Israelsson LA (2009) Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Arch Surg 144:1056–1059
Bosanquet DC, Ansel J, Abdelrahman T et al (2015) Systematic review and meta-regression of factors affecting midline incisional hernia rates: analysis of 14618 patients. PLoS One 10:e0138745
Deerenberg EB, Harlaar JJ, Steyerberg EW et al (2015) Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet 386:1254–1260
Osther PJ, Gjøde P, Mortensen BB, Mortenese PB, Bartholin J, Gottrup F (1995) Randomized comparison of polyglycolic acid and polyglyconate sutures for abdominal fascial closure after laparotomy in patients with suspected impaired wound healing. Br J Surg 82:1080–1082
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Additional information
S. Wang was a visiting scholar at Temple University School of Medicine now back at The First Municipal Hospital of Shijazhuang City, Hebei, China.
Rights and permissions
About this article
Cite this article
Guitarte, C., Grant, J., Zhao, H. et al. Incisional hernia formation and associated risk factors on a gynecologic oncology service: an exploratory analysis. Arch Gynecol Obstet 294, 805–811 (2016). https://doi.org/10.1007/s00404-016-4100-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4100-3