Abstract
Purpose
The present study investigated whether fibrinogen level during the first stage of labor is associated with bleeding severity in the third stage of labor.
Methods
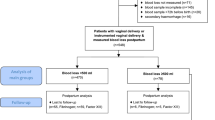
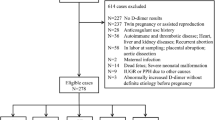
We prospectively enrolled 1019 pregnant women with planned vaginal delivery. Upon admission to delivery, maternal fibrinogen levels, hemoglobin content, and coagulation parameters were evaluated. Blood loss in the third stage of labor was systematically measured using a calibrated collecting drape. Univariate and multivariate analyses were performed to identify predictors of PPH (blood loss ≥500 mL) and S-PPH (blood loss ≥1000 mL).
Results
Among 809 vaginal deliveries, mean maternal predelivery fibrinogen was 4.65 ± 0.77 g/L, PPH incidence was 12 %, S-PPH incidence was 3.5 %, and median blood loss was 250 mL. Fibrinogen levels were significantly lower in women with S-PPH (4.22 ± 0.82 g/L) than without S-PPH (4.67 ± 0.75 g/L; p = 0.004), but did not significantly differ between women with PPH (4.67 ± 0.84 g/L) and those without PPH (4.67 ± 0.75 g/L; p = 0.985). Instrumental delivery and predelivery fibrinogen levels were independent predictors of S-PPH. Primiparous status, birth weight >4000 g, genital tract laceration, episiotomy and instrumental delivery were independent predictors of PPH.
Conclusion
For each 1 g/L increase of predelivery fibrinogen level, the risk of S-PPH after vaginal delivery decreases by a factor of 0.405 (95 % CI 0.219–0.750; p = 0.004).

Similar content being viewed by others
References
Khan KS, Wojdyla D, Say L et al (2006) WHO analysis of causes of maternal death: a systematic review. Lancet 367(9516):1066–1074. doi:10.1016/S0140-6736(06)68397-9 (published online first: epub date)
Bouwmeester FW, Bolte AC, van Geijn HP (2005) Pharmacological and surgical therapy for primary postpartum hemorrhage. Curr Pharm Des 11(6):759–773
Tunçalp O, Souza JP, Gülmezoglu M et al (2013) New WHO recommendations on prevention and treatment of postpartum hemorrhage. Int J Gynaecol Obstet 123(3):254–256. doi:10.1016/j.ijgo.2013.06.024 (published online first: epub date)
Gynecologists ACoOa (2006) ACOG practice bulletin: clinical management guidelines for obstetrician–gynecologists number 76, October 2006: postpartum hemorrhage. Obstet Gynecol 108(4):1039–1047
Henrich W, Surbek D, Kainer F et al (2008) Diagnosis and treatment of peripartum bleeding. J Perinat Med 36(6):467–478. doi:10.1515/JPM.2008.093 (published online first: epub date)
Bose P, Regan F, Paterson-Brown S (2006) Improving the accuracy of estimated blood loss at obstetric haemorrhage using clinical reconstructions. BJOG 113(8):919–924. doi:10.1111/j.1471-0528.2006.01018.x (published online first: epub date)
Prasertcharoensuk W, Swadpanich U, Lumbiganon P (2000) Accuracy of the blood loss estimation in the third stage of labor. Int J Gynaecol Obstet 71(1):69–70
Biguzzi E, Franchi F, Ambrogi F et al (2012) Risk factors for postpartum hemorrhage in a cohort of 6011 Italian women. Thromb Res 129(4):e1–e7. doi:10.1016/j.thromres.2011.09.010 (published online first: epub date)
Briley A, Seed PT, Tydeman G et al (2014) Reporting errors, incidence and risk factors for postpartum haemorrhage and progression to severe PPH: a prospective observational study. BJOG 121(7):876–888. doi:10.1111/1471-0528.12588 (published online first: epub date)
Peyvandi F, Biguzzi E, Franchi F et al (2012) Elevated prepartum fibrinogen levels are not associated with a reduced risk of postpartum hemorrhage. J Thromb Haemost 10(7):1451–1453. doi:10.1111/j.1538-7836.2012.04755.x (published online first: epub date)
Charbit B, Mandelbrot L, Samain E et al (2007) The decrease of fibrinogen is an early predictor of the severity of postpartum hemorrhage. J Thromb Haemost 5(2):266–273. doi:10.1111/j.1538-7836.2007.02297.x (published online first: epub date)
Cortet M, Deneux-Tharaux C, Dupont C et al (2012) Association between fibrinogen level and severity of postpartum haemorrhage: secondary analysis of a prospective trial. Br J Anaesth 108(6):984–989. doi:10.1093/bja/aes096 (published online first: epub date)
Clauss A (1957) Rapid physiological coagulation method in determination of fibrinogen. Acta Haematol 17(4):237–246
Organization WH (2012) WHO recommendations for the prevention and treatment of postpartum haemorrhage
Schlembach D, Mörtl MG, Girard T et al (2014) Management of postpartum hemorrhage (PPH): algorithm of the interdisciplinary D-A-CH consensus group PPH (Germany–Austria–Switzerland). Anaesthesist 63(3):234–242. doi:10.1007/s00101-014-2291-1 (published online first: epub date)
Karlsson O, Jeppsson A, Thornemo M et al (2015) Fibrinogen plasma concentration before delivery is not associated with postpartum haemorrhage: a prospective observational study. Br J Anaesth. doi:10.1093/bja/aev039 (published online first: epub date)
Yamada T, Akaishi R, Oda Y et al (2014) Antenatal fibrinogen concentrations and postpartum haemorrhage. Int J Obstet Anesth 23(4):365–370. doi:10.1016/j.ijoa.2014.06.004 (published online first: epub date)
Zhang WH, Deneux-Tharaux C, Brocklehurst P et al (2010) Effect of a collector bag for measurement of postpartum blood loss after vaginal delivery: cluster randomised trial in 13 European countries. BMJ 340:c293
Szecsi PB, Jørgensen M, Klajnbard A et al (2010) Haemostatic reference intervals in pregnancy. Thromb Haemost 103(4):718–727. doi:10.1160/TH09-10-0704 (published online first: epub date)
Abbassi-Ghanavati M, Greer LG, Cunningham FG (2009) Pregnancy and laboratory studies: a reference table for clinicians. Obstet Gynecol 114(6):1326–1331. doi:10.1097/AOG.0b013e3181c2bde8 (published online first: epub date)
Bremme KA (2003) Haemostatic changes in pregnancy. Best Pract Res Clin Haematol 16(2):153–168
Uchikova EH, Ledjev II (2005) Changes in haemostasis during normal pregnancy. Eur J Obstet Gynecol Reprod Biol 119(2):185–188. doi:10.1016/j.ejogrb.2004.06.038 (published online first: epub date)
de Lloyd L, Bovington R, Kaye A et al (2011) Standard haemostatic tests following major obstetric haemorrhage. Int J Obstet Anesth 20(2):135–141. doi:10.1016/j.ijoa.2010.12.002 (published online first: epub date)
Gayat E, Resche-Rigon M, Morel O et al (2011) Predictive factors of advanced interventional procedures in a multicentre severe postpartum haemorrhage study. Intensive Care Med 37(11):1816–1825. doi:10.1007/s00134-011-2315-0 (published online first: epub date)
Bell SF, Rayment R, Collins PW et al (2010) The use of fibrinogen concentrate to correct hypofibrinogenaemia rapidly during obstetric haemorrhage. Int J Obstet Anesth 19(2):218–223. doi:10.1016/j.ijoa.2009.08.004 (published online first: epub date)
Mercier FJ, Bonnet MP (2010) Use of clotting factors and other prohemostatic drugs for obstetric hemorrhage. Curr Opin Anaesthesiol 23(3):310–316. doi:10.1097/ACO.0b013e32833835a2 (published online first: epub date)
Mallaiah S, Barclay P, Harrod I et al (2015) Introduction of an algorithm for ROTEM-guided fibrinogen concentrate administration in major obstetric haemorrhage. Anaesthesia 70(2):166–175. doi:10.1111/anae.12859 (published online first: epub date)
Wikkelsø AJ, Edwards HM, Afshari A et al (2015) Pre-emptive treatment with fibrinogen concentrate for postpartum haemorrhage: randomized controlled trial. Br J Anaesth 114(4):623–633. doi:10.1093/bja/aeu444 (published online first: epub date)
Ramanathan G, Arulkumaran S (2006) Postpartum hemorrhage. J Obstet Gynaecol Can 28(11):967–973
Ekin A, Gezer C, Solmaz U et al (2015) Predictors of severity in primary postpartum hemorrhage. Arch Gynecol Obstet 292(6):1247–1254. doi:10.1007/s00404-015-3771-5 (published online first: epub date)
Al-Zirqi I, Vangen S, Forsen L et al (2008) Prevalence and risk factors of severe obstetric haemorrhage. BJOG 115(10):1265–1272. doi:10.1111/j.1471-0528.2008.01859.x (published online first: epub date)
Bais JM, Eskes M, Pel M et al (2004) Postpartum haemorrhage in nulliparous women: incidence and risk factors in low and high risk women. A Dutch population-based cohort study on standard (≥500 ml) and severe (≥1000 ml) postpartum haemorrhage. Eur J Obstet Gynecol Reprod Biol 115(2):166–172. doi:10.1016/j.ejogrb.2003.12.008 (published online first: epub date)
Sheiner E, Sarid L, Levy A et al (2005) Obstetric risk factors and outcome of pregnancies complicated with early postpartum hemorrhage: a population-based study. J Matern Fetal Neonatal Med 18(3):149–154. doi:10.1080/14767050500170088 (published online first: epub date)
Helman S, Drukker L, Fruchtman H et al (2015) Revisit of risk factors for major obstetric hemorrhage: insights from a large medical center. Arch Gynecol Obstet 292(4):819–828. doi:10.1007/s00404-015-3725-y (published online first: epub date)
Conner SN, Tuuli MG, Colvin R et al (2015) Accuracy of estimated blood loss in predicting need for transfusion after delivery. Am J Perinatol. doi:10.1055/s-0035-1552940 (published online first: epub date)
Oyelese Y, Ananth CV (2010) Postpartum hemorrhage: epidemiology, risk factors, and causes. Clin Obstet Gynecol 53(1):147–156. doi:10.1097/GRF.0b013e3181cc406d (published online first: epub date)
Acknowledgments
We would like to thank the obstetric team of our department for helping to enroll patients and to measure blood loss after childbirth. We thank Andrea Ernert for kindly providing useful statistical support and Aarne Feldheiser and Michaela Kolbe for their friendly and helpful advices.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
K. Niepraschk-von Dollen and C. Bamberg contributed equally.
Rights and permissions
About this article
Cite this article
Niepraschk-von Dollen, K., Bamberg, C., Henkelmann, A. et al. Predelivery maternal fibrinogen as a predictor of blood loss after vaginal delivery. Arch Gynecol Obstet 294, 745–751 (2016). https://doi.org/10.1007/s00404-016-4031-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4031-z