Abstract
Introduction
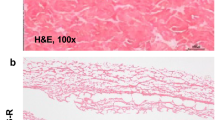
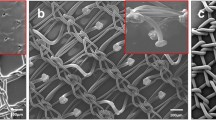
Differences in mesh composition may affect outcomes such as erosion, tissue integration and inflammation. The majority of commercially available meshes are type 1, manufactured from monofilament polypropylene with differing pore sizes and mechanical properties.
Objective
To assess the local tolerance of four commercially available meshes in terms of mesh integration and host tissue response.
Method
Using an animal model, mesh was implanted onto the abdominal sheath. Animals were sacrificed at 7, 30 and 90 days and data collected.
Results
Strength of mesh-skin integration increased in all groups across the three time points. Polyform displayed highest strength of separation overall. VM PFR and Iprolite reached their maximum integration earliest. In regard to mesh abdominal wall integration Polyform had the greatest strength of separation, with Ultrapro displaying some weakening of integration at 30 and 90 days. Host tissue response was similar in all groups at each time point.
Conclusion
Polyform and VM PFR have enhanced tissue integration when compared to Ultrapro. This decreased integration in Ultrapro may lead to increased mesh failure. The composition of mesh affects its integration and potentially its failure rate but not host tissue response. These observations in mesh characteristics may benefit the design of next generation meshes with a view to reducing failure rates and erosion.








Similar content being viewed by others
References
Subak LL et al (2001) Cost of pelvic organ prolapse surgery in the United States. Obstet Gynecol 98(4):646–651
Olsen AL et al (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89(4):501–506
Cordozo L (1995) Urinary incontinence. In: Whitfield CR (ed) Dewhursts textbook of obstetrics and gynaecology for postgraduates. Blackwell Science, Oxford, pp 642–652
Brown JS et al (2002) Pelvic organ prolapse surgery in the United States, 1997. Am J Obstet Gynecol 186(4):712–716
Maher C et al (2008) Surgical management of pelvic organ prolapse in women: a short version Cochrane review. Neurourol Urodyn 27(1):3–12
Birch C, Fynes MM (2002) The role of synthetic and biological prostheses in reconstructive pelvic floor surgery. Curr Opin Obstet Gynecol 14(5):527–535
Usher FC (1962) Hernia repair with Marlex mesh. An analysis of 541 cases. Arch Surg 84:325–328
Cumberland VH (1952) A preliminary report on the use of prefabricated nylon weave in the repair of ventral hernia. Med J Aust 1(5):143–144
Scales JT (1953) Tissue reactions to synthetic materials. Proc R Soc Med 46(8):647–652
Amid PK, Lichtenstein IL (1996) Retromuscular alloplasty of large scar hernias: a simple staple attachment technique. Chirurg 67(6):648–652
White RA (1988) The effect of porosity and biomaterial on the healing and long-term mechanical properties of vascular prostheses. ASAIO Trans 34(2):95–100
Usher FC et al (1962) Polypropylene monofilament. A new, biologically inert suture for closing contaminated wounds. JAMA 179:780–782
Bauer JJ et al (1987) Repair of large abdominal wall defects with expanded polytetrafluoroethylene (PTFE). Ann Surg 206(6):765–769
Pans A et al (2001) Biochemical study of collagen in adult groin hernias. J Surg Res 95(2):107–113
Afonso JS et al (2009) Structural and thermal properties of polypropylene mesh used in treatment of stress urinary incontinence. Acta Bioeng Biomech 11(3):27–33
Dietz HP et al (2003) Mechanical properties of urogynecologic implant materials. Int Urogynecol J Pelvic Floor Dysfunct 14(4):239–243 discussion 243
Gabriel B et al (2011) Vagina, abdominal skin, and aponeurosis: do they have similar biomechanical properties? Int Urogynecol J Pelvic Floor Dysfunct 22(1):23–27
Haylen BT et al (2011) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Neurourol Urodyn 30(1):2–12
Haylen BT et al (2011) An international urogynecological association (IUGA)/international continence society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Int Urogynecol J Pelvic Floor Dysfunct 22(1):3–15
Brubaker L, Bump RC, Fynes M (2005) Surgery for plevic organ prolapse. In: Abrams P, Cardozo L, Koury S, Weins A (eds) Third International consultation on incontinence, 1st edn. Health publication, Plymouth
Neel HB 3rd (1983) Implants of gore-tex. Arch Otolaryngol 109(7):427–433
Soler M et al (1993) Treatment of postoperative incisional hernias by a composite prosthesis (polyester-polyglactin 910). Clinical and experimental study. Ann Chir 47(7):598–608
Collaboration TEHT (2000) Mesh compared with non-mesh methods of open groin hernia repair: systematic review of randomized controlled trials. Br J Surg 87(7):854–859
Cervigni M, Natale F (2001) The use of synthetics in the treatment of pelvic organ prolapse. Curr Opin Urol 11(4):429–435
Conflict of interest
This study was co-sponsored by Boston Scientific Corporation and Proxy Biomedical Limited. Dr O’Reilly acts as an advisor to Proxy Biomedical Limited, with no financial benefit.
Ethical approval
The study was granted ethical approval using Institutional Animal Care and Use Committee (IACUC) protocol number 2006-0147 at Case Western Reserve University, Cleveland, Ohio, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O’Sullivan, O.E., Connor, J. & O’Reilly, B.A. Lightweight meshes: evaluation of mesh tissue integration and host tissue response. Arch Gynecol Obstet 289, 1029–1037 (2014). https://doi.org/10.1007/s00404-013-3093-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-013-3093-4