Abstract
Purpose
To model the timing and sequence of intrapartum interventions and to estimate the association with labor length and delivery mode.
Methods
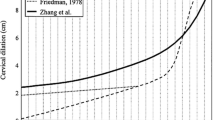
A longitudinal multi-center cohort study included data from 3,955 low-risk women who gave birth in hospitals in Lower Saxony, Germany. We analyzed three intrapartum interventions: amniotomy, oxytocin augmentation and epidural analgesia. We divided births into time intervals delineated by these interventions and noted cervical dilation at interval onset. We analyzed the duration of intervals from onset of labor until the first intervention and between intrapartum interventions with Kaplan–Meier’s estimate, regarding the three interventions as competing risks. Further, we analyzed the cervical dilation before an intervention by Kaplan–Meier’s estimate without censoring.
Results
73.2 % of the included 2,082 nulliparae (n = 1,525) and 59.6 % of the included 1,873 multiparae (n = 1,117) received at least one intervention, while 1,313 women (33.2 %) experienced a normal labor without any of these interventions. The intervals from onset of labor until the first intervention and from the first until the second intervention were significantly shorter in multiparae than in nulliparae. The intervention cascade in nulliparae most often started with epidural analgesia in early labor (n = 579, 27.8 %). Oxytocin augmentation most often followed after a short interval (n = 343, 59.2 %, median 1.57 h). In multiparae, amniotomy was most often the first intervention (n = 629, 33.6 %), and spontaneous birth most often followed (n = 503, 80.0 %). Labor duration and operative deliveries increased as interventions increased.
Conclusions
The temporal sequence of intrapartum interventions varied in association with parity, cervical dilation, labor duration and mode of birth.



Similar content being viewed by others
References
Anim-Somuah M, Smyth RMD, Jones L (2011) Epidural versus non-epidural or no analgesia in labor. Cochrane Database Syst Rev 4:CD000331. doi:10.1002/14651858.CD000331.pub3
Bakker PC, Kurver PH, Kuik DJ, Van Geijn HP (2007) Elevated uterine activity increases the risk of fetal acidosis at birth. Am J Obstet Gynecol 196:313.e1–6
Bugg GJ, Siddiqui F, Thornton JG (2011) Oxytocin versus no treatment or delayed treatment for slow progress in the first stage of spontaneous labour. Cochrane Database Syst Rev 7:CD007123. doi:10.1002/14651858.CD007123.pub2
Clark S, Belfort M, Saade G et al (2007) Implementation of a conservative checklist-based protocol for oxytocin administration: maternal and newborn outcomes. Am J Obstet Gynecol 197:480.e1–5
Clark SL, Simpson KR, Knox GE, Garite TJ (2009) Oxytocin: new perspectives on an old drug. Am J Obstet Gynecol 200:35.e1–6
Costley PL, East CE (2012) Oxytocin augmentation of labour in women with epidural analgesia for reducing operative deliveries. Cochrane Database Syst Rev 5:CD009241. doi:10.1002/14651858.CD009241.pub2
Dickinson JE, Godfrey M, Evans SF, Newnham JP (1997) Factors influencing the selection of analgesia in spontaneously labouring nulliparous women at term. Aust N Z J Obstet Gynaecol 37:289–293
German Society of Obstetrics and Gynecology (DGGG) (2008) Pre-and peripartum care in women with status post cesarean section. http://www.dggg.de/fileadmin/public_docs/Leitlinien/3-4-5-entbindung-nach-sectio-2010.pdf. Accessed 23 Dec 2010
German Society of Obstetrics and Gynaecology (DGGG) (2008) Tocolytics to prevent preterm birth. AWMF 015/025. http://www.dggg.de/leitlinien/aktuelle-leitlinien/. Accessed 23 Dec 2010
Hawkins JL (2010) Epidural analgesia for labor and delivery. N Engl J Med 362:1503–1508
Leighton BL, Halpern SH (2002) Epidural analgesia: effects on labor progress and maternal and neonatal outcome. Semin Perinatol 26:122–135
Latouche A, Beyersmann J, Fine JP (2007) Comments on ‘analysing and interpreting competing risk data’. Stat Med 26:3676–3679
Lok J (2008) Statistical modeling of causal effects in continuous time. Ann Stat 36:1464–1507
Ohel G, Gonen R, Vaida S, Barak S, Gaitini L (2006) Early versus late initiation of epidural analgesia in labor: does it increase the risk of cesarean section? A randomized trial. Am J Obstet Gynecol 194:600–605
Pintilie M (2007) Analysing and interpreting competing risk data. Stat Med 26:1360–1367
Petersen A, Ayerle GM, Frömke C, Hecker H, Gross MM (2011) The timing of interventions during labour: descriptive results of a longitudinal study. Midwifery 27(6):e267–e273. doi:10.1016/j.midw.2010.10.017
Rahm VA, Hallgren A, Högberg H, Hurtig I, Odlind V (2002) Plasma oxytocin levels in women during labor with or without epidural analgesia: a prospective study. Acta Obstet Gynecol Scand 81:1033–1039
Roberts CL, Algert CS, Douglas I, Tracy SK, Peat B (2002) Trends in labour and birth interventions among low-risk women in New South Wales. Aust N Z J Obstet Gynaecol 42:176–181
Rooks JP (2009) Oxytocin as a “high alert medication”: a multilayered challenge to the status quo. Birth 36:345–348
Selin L, Almström E, Wallin G, Berg M (2009) Use and abuse of oxytocin for augmentation of labor. Acta Obstet Gynecol Scand 88:1352–1357
Simpson KR, James DC (2008) Effects of oxytocin-induced uterine hyperstimulation during labor on fetal oxygen status and fetal heart rate patterns. Am J Obstet Gynecol 199:34.e1–5
Smyth RM, Alldred SK, Markham C (2007) Amniotomy for shortening spontaneous labour. Cochrane Database Syst Rev 4:CD006167. doi:10.1002/14651858.CD006167.pub2
Tracy SK, Sullivan E, Wang YA, Black D, Tracy M (2007) Birth outcomes associated with interventions in labour amongst low risk women: a population-based study. Women Birth 20:41–48
Wei SQ, Luo ZC, Xu H, Fraser WD (2009) The effect of early oxytocin augmentation in labor: a meta-analysis. Obstet Gynecol 114:641–649
Wei S, Wo BL, Xu H, Luo ZC, Roy C, Fraser WD (2009) Early amniotomy and early oxytocin for prevention of or therapy for, delay in first stage spontaneous labour compared with routine care. Cochrane Database Syst Rev 2:CD006794. doi:10.1002/14651858.CD006794.pub2
Acknowledgments
The study was funded by the German Research Council (DFG).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Petersen, A., Poetter, U., Michelsen, C. et al. The sequence of intrapartum interventions: a descriptive approach to the cascade of interventions. Arch Gynecol Obstet 288, 245–254 (2013). https://doi.org/10.1007/s00404-013-2737-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-013-2737-8