Abstract
Purpose
Hysterosalpingography (HSG) is an important tool for evaluation of tubal factors in infertility. It does not require anesthesia but can be a painful procedure. Thus, this study was undertaken to establish the role of intracervical block as pain relief modality for HSG.
Methods
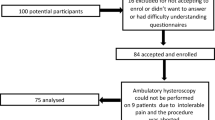
This prospective, randomized study included hundred women attending the Department of Obstetrics and Gynecology, at a tertiary care centre in India. They were divided randomly through a computer generated table into two groups of 50 women each. In the study group, women received intracervical block along with premedication whereas in the control group women received premedication alone. Each patient was asked to rate her pain at six different points of time (T1–T6) during HSG using Visual analogue scale (VAS) and Verbal descriptive score. The difference in pain scores amongst the two groups was analyzed using independent t test.
Results
Reduction of pain was observed from placement of tenaculum till end of procedure (T3–T6) with intracervical block (p < 0.05). Pain remained at a statistically lower level during the most painful steps i.e. traction of the cervix (VAS: 2.080.49 cm, 95 % C I 1.18–2.98 vs. 4.21.15 cm, 95 % CI 3.3–5.1, p = 0.001) and with the insertion of dye (VAS: 2.640.49, 95 % CI 1.7–3.5 vs. 5.121.45. 95 % CI 4.3–6.0, p = 0.001) in the study group as compared to control group.
Conclusion
Intracervical block can be offered to all women undergoing HSG to make the procedure less painful and thus improve the compliance.
Similar content being viewed by others
References
Hull MG, Glazener CM, Kelly NJ, Conway DI, Foster PA, Hinton RA et al (1985) Population study of causes, treatment and outcome of infertility. Br Med J 291:1693–1697
Taylor A (2003) ABC of subfertility making a diagnosis. BMJ 327:494–497
Mol BW, Collins JA, Burrows EA, van der Veen F, Bossuyt PM (1999) Comparison of hysterosalpingography and laparoscopy in predicting fertility outcome. Hum Reprod 14:1237–1242
Ayida G, kennedy S, Barlow D, Chamberlain P (1996) A comparison of patient tolerance of hysterosalpingography-contrast-sonography (HyCoSy) with Echovist-200 and X-ray hysterosalpingography for outpatient investigation of infertile women. Ultrasound Obstet Gynecol 7:201–204
Moore DE, Pain associated hysterosalpingography (1985) Ethiodol versus salpinx media. Fertil Steril 38:629–631
Owens OM, Schiff I, Kaul AF, Cramer DC, Burt RA (1985) Reduction of pain following hysterosalpingogram by prior analgesic administration. Fertil Steril 43:146–148
Elson EM, Ridley NT (2000) Paracetamol as a prophylactic analgesic for hysterosalpingography: a double blind randomized controlled trial. Clin Radiol 55:675–678
Lorino CO, Prough SG, Aksel S, Abuzeid M, Alexander SE, Wiebe RH (1990) Pain relief in hysterosalpingography: a comparison of analgesics. J Reprod Med 35:533–536
Costello MF, Horrowitz S, Steigrad S, Saif N, Bennett M, Ekangaki A (2002) Transcervical intrauterine topical local anesthetic at hysterosalpingography: a prospective, randomized, double-blind, placebo-controlled trial. Fertil Steril 78:1116–1122
Wiebe ER (1992) Comparison of the efficacy of different local anesthetics and techniques of local anesthesia in therapeutic abortions. Am J Obstet Gynecol 167:131–134
Cicinelli E, Didonna T, Schonauer LM, Stragapede S, Falco N, Pansini N (1998) Paracervical anesthesia for hysteroscopy and endometrial biopsy in postmenopausal women: a randomized, double blind, placebo controlled study. J Reprod Med 43:1014–1018
Ezeh UO (1995) Outpatient hysteroscopy: paracervical block. Fertil Steril 64:221–222
Rosen MA (2002) Paracervical block for labor analgesia: a brief historic review. Am J Obstet Gynecol 186(5):127–130
Robinson RD, Casablanca Y, Pagano KE, Arthur NA, Bates GW, Propst AM (2007) Intracervical block and pain perception during the performance of a hysterosalpingogram – a randomized controlled trial. Am J Obstet Gynaecol 109:89–93
Gupta N, Sharma JB, Mittal S, Singh N, Misra R, Kukreja M (2007) Genital tuberculosis in Indian infertility patients. Int J Gynecol Obstet 97(2):135–138
Chapman CR, Syrjala K (1990) Measurement of pain. In: Bonica JJ (ed) The management of pain, 2nd edn. Lea and Febiger, Philadelphia, pp 580–594
Huskisson EC (1974) Measurement of pain. Lancet 2:1127–1131
Ware J, Epps C, Herr K, Packard A (2006) Evaluation of the revised faces pain scale, verbal descriptive scale, numeric rating scale and lowa pain thermometer in older minority adults. Pain Mgt Nurs 7:117–125
NICE (2004) Fertility: assessment and treatment for people with fertility problems. NICE guidelines
Collins SL, Moore RA, McQuay HJ (1997) The visual analog pain intensity scale: what is moderate pain in millimeters. Pain 72:95–97
Liberty G, Gal M, Mazaki E, Eldar-Geva T, Vatashsky E, Margalioth EJ (2005) Pain relief of hysterosalpingography by prior uterine cervical application of lidocaine/prilocaine cream. Fertil Steril 84:127–128
Hamed HO, Shahim AY, Elsamman AM (2009) Hystersalpingo-contrast-sonography versus radiography in the evaluation of tubal patency. Int J Gynecol Obstet 105(3):215–217
Stacey C, Bown C, Manhire A, Rose D (2000) Hy-Co-Sy-as good as claimed? Br J Radiol 73:133–136
Scolov D, Boran I, Boiculese L, Tamba B, Anghelache-Lupascu I, Socolov R (2010) Comparison of the pain experienced by infertile women undergoing hysterosalpingo contrast sonography or radiographic hysterosalpingography. Int J Gynaecol Obstet 111(3):256–259
Saunder Riana D, Shwayder James M, Nakajima Steven T (2011) Current methods of tubal patency assessment. Fertil Steril 95(7):2171–2179
Ahinko- Hakamaa K, Huhtala H, Ttinkanen H (2007) The validity of air & saline HYy-Co-Sy in tubal patency investigation before insemination treatment. Eur J Obstet Gynecol Reprod Biol 132:83–87
Lim CP, Hasafa Z, Bhattacharya S, Maheshwari A (2011) Should a hysterosalpingogram be a first-line investigation to diagnose female tubal subfertility in the modern subfertility workup? Hum Reprod 26(5):967–971
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chauhan, M.B., Lakra, P., Jyotsna, D. et al. Pain relief during hysterosalpingography: role of intracervical block. Arch Gynecol Obstet 287, 155–159 (2013). https://doi.org/10.1007/s00404-012-2515-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-012-2515-z