Abstract
Purpose
The aim of the study was to evaluate disease persistence after conization of CIN3 and microinvasive cervical carcinoma.
Methods
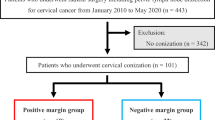
Medical records from a total of 231 patients were reviewed. The prevalence of CIN3 and cervical carcinoma diagnosed by means of conization were analyzed. All conizations were performed under lumbar anesthesia using a laser technique.
Results
Of the 231 patients, 25 had margin involvement with CIN3 or microinvasive carcinoma. Among these 25 patients, 10 underwent hysterectomy. Two of these 10 patients had CIN3 and eight had microinvasive carcinoma. Residual disease was observed in hysterectomy specimens from 9 of the 10 patients. Of the eight patients diagnosed with microinvasion from post-cone hysterectomy specimens, four had CIN3 and three had microinvasive carcinoma. The three patients with microinvasion were found to have a larger area of residual disease as compared with other patients with margin involvement.
Conclusions
Conization alone seems to be a reasonable treatment for patients with CIN1, 2, 3, and microinvasive carcinoma. For adenocarcinoma, in situ treatment with conization alone is possible but requires careful follow-up. Hysterectomy appears to be a safe treatment option for microinvasive adenocarcinoma, although follow-up by cytology is sometimes possible in cases with negative surgical margins.
Similar content being viewed by others
References
Ostor AG (1993) Natural history of cervical intraepithelial neoplasia: a critical review. Int J Gynecol Pathol 12:186–192
Bigrigg A, Haffenden DK, Sheehan AL, Codling BW, Read MD (1994) Efficacy and safety of large-loop excision of the transformation zone. Lancet 343:32–34
Tabor A, Berget A (1990) Cold-knife and laser conization for cervical intraepithelial neoplasia. Obstet Gynecol 76:633–635
Arbyn M, Kyrgiou M, Martin-Hirsch P, Prendiville W, Paraskevaidis E (2008) Perinatal mortality and other severe adverse pregnancy outcomes associated with treatment of cervical intraepithelial neoplasia: meta-analysis. BMJ 337:a1284
Prendiville W (2009) The treatment of CIN: what are the risks? Cytopathology 20:145–153
Prendiville W, Cullimore J, Norman S (1989) Large loop excision of the transformation zone (LLETZ). A new method of management for women with cervical intra-epithelial neoplasia. Br J Obstet Gynaecol 96:1054–1060
Prendiville W (2003) LLETZ: theoretical rationale, practical aspects, clinical experience, optimizing the technique. In: Prendiville W, Tatti S, Ritter J, Twiggs L (eds) Colposcopy: Management Options Ch10. Saunders, Philadelphia WB
Prendiville W (2003) Excision of the transformation zone. In: Maclean A, Singer A, Critchley H (eds) Lower Genital Tract Neoplasia. RCOG Press, London, pp 179–188
Reich O, Lahousen M, Pickel H, Tamussino K, Winter R (2002) Cervical intraepithelial neoplasia III: long-term follow-up after cold-knife conization with involved margins. Obstet Gynecol 99:193–196
Monk A, Pushkin SF, Nelson AL, Gunning JE (1996) Conservative management of optional for patients with dysplasia involving endocervical margins of cervical cone biopsy specimens. Am J Obstet Gynecol 174:1695–1699
Tseng CJ, Horng SG, Soong TK, Hsueh S, Hsieh CH, Lin HW (1994) Conservative therapy for microinvasive carcinoma of the uterine cervix. Gynecol Oncol 53:109–113
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Sweeting MJ, Sutton AJ, Lambert PC (2004) What to add to nothing? Use and avoidance of continuity corrections in meta-analysis of sparse data. Stat Med 23:1351–1375
Costa S, De Nuzzo M, Infante FE, Bonavita B, Marinelli M, Rubino A, Rambelli V, Santini D, Cristiani P, Bucchi L (2002) Disease persistence in patients with cervical intraepithelial neoplasia undergoing electrosurgical conization. Gynecol Oncol 85:119–124
Paraskevaidis E, Koliopoulos G, Malamou-Mitsi V, Zikopoulos K, Paschopoulos M, Pappa L, Agnantis NJ, Loli DE (2001) Large loop excision of the transformation zone for treating cervical intraepithelial neoplasia: a 12-year experience. Anticancer Res 21:3097–3099
Lopes A, Morgan P, Murdoch J, Piura B, Monaghan JM (1993) The case for conservative management of “incomplete excision” of CIN after laser conization. Gynecol Oncol 49:247–249
Lapaquette TK, Dinh TV, Hannigan EV, Doherty MG, Yandell RB, Buchanan VS (1993) Management of patients with positive margins after cervical conization. Obstet Gynecol 82:440–443
Itsukaichi M, Kurata H, Matsushita M, Watanabe M, Sekine M, Aoki Y, Tanaka K (2003) Stage Ia1 cervical squamous cell carcinoma: conservative management after laser conization with positive margins. Gynecol Oncol 90:387–389
Lee SJ, Kim WY, Lee JW, Kim HS, Choi TL, Ahn GH, Lee JH, Kim BG, Bae DS (2009) Conization using electrosurgical conization and cold coagulation for international federation of gynecology and obstetrics stage IA1 squamous cell carcinomas of the uterine cervix. Int J Gynecol Cancer 19:407–411
Salani R, Puri I, Bristow RE (2009) Adenocarcinoma in situ of the uterine cervix: a metaanalysis of 1278 patients evaluating the predictive value of conization margin status. Am J Obstet Gynecol 200:182
Delgado G, Bundy B, Zaino R, Sevin BU, Creasman WT, Major F (1990) Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol 38:352–357
Conflict of interest
We declare that we have no conflicts of interest in connection with this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takeda, N., Suzuki, T., Suzuki, M. et al. Evaluation of cervical conization as a definitive treatment for microinvasive cervical carcinoma and cervical intraepithelial neoplasia grade 3. Arch Gynecol Obstet 285, 453–457 (2012). https://doi.org/10.1007/s00404-011-1944-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-011-1944-4