Abstract
Objective
The formation of cysts during IVF treatment may negatively influence the outcome. The aim of this study is to compare conservative management versus aspiration for functional ovarian cysts before ovarian stimulation for ART.
Materials and methods
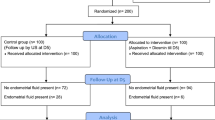
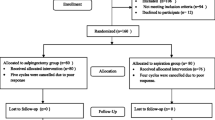
Women who underwent IVF cycle with a long protocol, and developed ovarian cysts, they were randomly divided into a cyst aspiration group (n = 90) in which the cysts were aspirated after diagnosis and a no-intervention group (n = 90) for which the conservative treatment was continued following cyst diagnosis.
Results
The FSH level in women with ovarian cysts in the aspiration group was significantly higher than that in the no-intervention group (9.1 ± 4.5 vs. 6.5 ± 1.78 mIU/ml, p = 0.001). HMG requirement in that aspiration group was significantly higher than that in the non- intervention group (26.2 ± 9.7 vs. 21.85 ± 7.7, p = 0.0001). The embryo score in the no-intervention group was higher than the aspiration group (18 vs. 16, p = 0.0001).The cycle cancellation rate was significantly higher in the aspiration group than the no-intervention group. The pregnancy rate was higher but not significantly in the aspiration group than no-intervention group.
Conclusion
Cyst aspiration did not promote retrieved oocyte in quality and in number. Because cyst aspiration requires anesthesia and is expensive, conservative management is better and without improving the IVF outcome.
Similar content being viewed by others
References
Orvieto R, Zohav E, Scharf S, Rabinson J, Meltcer S, Anteby EY, Homburg R (2007) The influence of estradiol/follicle and estradiol/oocyte ratios on the outcome of controlled ovarian stimulation for in vitro fertilization. Gynecol Endocrinol 23(2):72–75
Ku SY, Choi YS, Jee BC, Suh CS, Choi YM, Kim JG, Moon SY, Kim SH (2005) A preliminary study on reduced dose (33 or 25 microg) gonadotropin-releasing hormone agonist long protocol for multifollicular ovarian stimulation in patients with high basal serum follicle-stimulating hormone levels undergoing in vitro fertilization-embryo transfer. Gynecol Endocrinol 21(4):227–231
Speroff L, Fritz MA (2005) Clinical gynecology endocrinology and infertility
Liu HC, Lai YM, Davis O, Berkeley AS, Graf M, Grifo J, Cohen J, Rosenwaks Z (1992) Improved pregnancy outcome with gonadotropin releasing hormone agonist (GnRH-a) stimulation is due to the improvement in oocyte quantity rather than quality. J Assist Reprod Genet 9(4):338–344
Jenkins JM, Davies DW, Anthony F, Wood P, Gadd SG, Waston RH (1992) The detrimental influence of functional ovarian cyst during in vitro fertilization cycles. Human Reprod 7:776–780
Jenkins JM, Davies DW, Anthony F, Wood P, Rushen D, Masson GM, Thomas E (1993) The development of functional ovarian cyst during pituitary down regulation. Hum Reprod 8:1623–1627
Feldburg D, Dicker D, Yeshaya A (1989) Ovarian cyst formation: a complication of gonadotropin-relasing hormone agonist therapy. Fertil Steril 51:42–44
Fiszbajn GE, Lipowicz RG, Elberger L, Grabia A, Dapier SD, Brugo-Olmedo SP (2000) Conservative management versus aspiration of functional ovarian cyst before ovarian stimulation for assisted reproduction. J Assisted Reprod Genet 17:206–263
Herman A, Ron-EI R, Golan A, Capsie E (1990) Follicle cysts after menstrual versus mid luteal administration of gonadotropin-releasing hormone in vitro fertilization. Fertil Steril 53:854–858
Biljan MM, Lapensec L, Mahutte NG, Bissonnette F, Hemmings R (2000) Effect of functional ovarian cysts detected on the 7th day of GnRH agonist administration on the outcome of IVF treatment. Fertil Steril 74:941–945
Qublan HS, Amarin Z, Tahat YA, Smadi AZ, Kilani M (2006) Ovarian cyst formation following GnRH agonist administration in IVF cycles: incidence and impact. Hum Reprod 21(3):640–644
Keltz MD, Jones EE, Duleba AJ, Polcz T, Kennedy K, Olive DL (1995) Baseline cyst formation after luteal phase gonadotropin-releasing hormone agonist administration is linked to poor in vitro fertilization outcome. Fertil Steril 64:568–572
Segal S, Shifren JL, Isaacson KB, Leykin L, Chang Y, Pal L, Toth TL (1999) Effect of a baseline ovarian cyst on the outcome of in vitro fertilization-embryo transfer. Fertil Steril 71(2):274–277
Owj M, Ashrafi M, Baghestani A (2004) Ovarian cyst formation and in vitro fertilization outcome. Int J Gynecol Obstet 87(3):258–259
Rizk B, Tan SL, Kingsland C, Steer C, Mason BA, Campbell S (1990) Ovarian cyst aspiration and outcome of in vitro fertilization. Fertil Steril 54:661–664
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Firouzabadi, R.D., Sekhavat, L. & Javedani, M. The effect of ovarian cyst aspiration on IVF treatment with GnRH. Arch Gynecol Obstet 281, 545–549 (2010). https://doi.org/10.1007/s00404-009-1195-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-009-1195-9