Abstract
Background
One of the most important hormones synthesized by the placenta during pregnancy is progesterone. The regulating mechanisms of progesterone synthesis and the mechanism responsible for the spontaneous onset of labor in women are still not fully understood. Progesterone is thought to have been involved in human parturition. The objective of this study was to compare the levels of progesterone in the human placentas, at the end of the gestation (37–41 weeks) in vaginal versus cesarean deliveries, and to evaluate the pattern of progesterone accumulation, instantly following its synthesis by the human placenta at the end of the pregnancy.
Methods
Progesterone levels in human placental tissue were determined by immunochemiluminescent analysis, following tissue homogenization. Progesterone secretion and accumulation pattern in the placental tissue was demonstrated using the ex vivo, closed, dual perfusion system of isolated human placental cotyledon.
Results
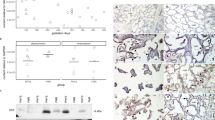
Immunochemiluminescent analysis of progesterone levels in human normal and cesarean-delivered placentas showed that placentas following normal vaginal delivery store higher concentrations of progesterone, and produce progesterone more intensively. Results obtained from 120-min perfusions (of vaginal and cesarean-delivered placentas) showed that progesterone tended to accumulate in the maternal rather than the fetal compartment.
Conclusions
These data indicate that progesterone levels continuously rise till the end of pregnancy, with no apparent drop in progesterone levels during the labor process. In addition, progesterone is released from the syncytiotrophoblast preferably into the maternal component of the placental tissue.


Similar content being viewed by others
References
Weier N, He SM, Li XT, Wang LL, Zhou SF (2008) Placental drug disposition and its clinical implications. Curr Drug Metab 9:106–121. doi:10.2174/138920008783571828
Skałba P, Dabkowska-Huć A, Chełmicki Z (2003) The endocrinology of the human placenta. Wiad Lek 56:475–480
Speroff L, Fritz MA (2005) Clinical gynecologic endocrinology and infertility, 7th edn. Lippincott Williams & Wilkins, Philadelphia
Denschlag D, Keck C (2002) The corpus luteum. Ther Umsch 59:159–162. doi:10.1024/0040-5930.59.4.159
Grow DR (2002) Metabolism of endogenous and exogenous reproductive hormones. Obstet Gynecol Clin North Am 29:425–436. doi:10.1016/S0889-8545(02)00009-8
Critchley HOD, Kelly RW, Brenner RM, Baird DT (2003) Antiprogestins as a model for progesterone withdrawal. Steroids 68:1061–1068. doi:10.1016/j.steroids.2003.07.001
Arck P, Hansen PJ, Mulac Jericevic B, Piccinni MP, Szekeres-Bartho J (2007) Progesterone during pregnancy: endocrine-immune cross talk in mammalian species and the role of stress. Am J Reprod Immunol 58:268–279. doi:10.1111/j.1600-0897.2007.00512.x
Tuckey RC (2005) Progesterone synthesis by the human placenta. Placenta 26:273–281. doi:10.1016/j.placenta.2004.06.012
Miyaura H, Iwata M (2002) Direct and indirect inhibition of Th1 development by progesterone and glucocorticoids. J Immunol 168:1087–1094
Shanker YG, Shetty UP, Rao AJ (1998) Regulation of low density lipoprotein receptor mRNA levels by estradiol 17beta and chorionic gonadotropin in human placenta. Mol Cell Biochem 187:133–139. doi:10.1023/A:1006843812495
Pasqualini JR (2005) Enzymes involved in the formation and transformation of steroid hormones in the fetal and placental compartments. J Steroid Biochem Mol Biol 97:401–415. doi:10.1016/j.jsbmb.2005.08.004
Bernal AL (2001) Overview of current research in parturition. Exp Physiol 86:213–222. doi:10.1113/eph8602178
Smith R (2007) Parturition. N Engl J Med 356:271–283. doi:10.1056/NEJMra061360
Mesiano S (2004) Myometrial progesterone responsiveness and the control of human parturition. J Soc Gynecol Investig 11:193–202. doi:10.1016/j.jsgi.2003.12.004
Thijssen JH (2005) Progesterone receptors in the human uterus and their possible role in parturition. J Steroid Biochem Mol Biol 97:397–400. doi:10.1016/j.jsbmb.2005.08.011
Mesiano S (2007) Myometrial progesterone responsiveness. Semin Reprod Med 25:5–13. doi:10.1055/s-2006-956771
Zakar T, Hertelendy F (2007) Progesterone withdrawal: key to parturition. Am J Obstet Gynecol 196:289–296. doi:10.1016/j.ajog.2006.09.005
Sheehan PM, Rice GE, Moses EK, Brennecke SP (2005) 5 Beta-dihydroprogesterone and steroid 5 beta-reductase decrease in association with human parturition at term. Mol Hum Reprod 11:495–501. doi:10.1093/molehr/gah201
Schneider H, Huch A (1985) Dual in vitro perfusion of an isolated lobe of human placenta: method and instrumentation. Contrib Gynecol Obstet 13:40–47
Myren M, Mose T, Mathiesen L, Knudsen LE (2007) The human placenta—an alternative for studying foetal exposure. Toxicol In Vitro 21:1332–1340. doi:10.1016/j.tiv.2007.05.011
Holcberg G, Sapir O, Tsadkin M, Huleihel M, Lazer S, Katz M, Mazor M, Ben-Zvi Z (2003) Lack of interaction of digoxin and P-glycoprotein inhibitors, quinidine and verapamil in human placenta in vitro. Eur J Obstet Gynecol Reprod Biol 109:133–137. doi:10.1016/S0301-2115(02)00513-4
Kopecky EA, Simone C, Knie B, Koren G (1999) Transfer of morphine across the human placenta and its interaction with naloxone. Life Sci 65:2359–2377. doi:10.1016/S0024-3205(99)00503-2
Shargel L, Cheung WM, Yu AB (1979) High-pressure liquid chromatographic analysis of antipyrine in small plasma samples. J Pharm Sci 68:1052–1054. doi:10.1002/jps.2600680835
Löfgren M, Bäckström T (1997) High progesterone is related to effective human labor. Study of serum progesterone and 5 alpha-pregnane-3, 20-dione in normal and abnormal deliveries. Acta Obstet Gynecol Scand 76:423–430. doi:10.3109/00016349709047823
Maynard PV, Stein PE, Symonds EM (1980) Umbilical cord plasma progesterone at term in relation to mode of delivery. Br J Obstet Gynaecol 87:864–868
Aisien AO, Towobola OA, Otubu JA, Imade GE (1994) Umbilical cord venous progesterone at term delivery in relation to mode of delivery. Int J Gynaecol Obstet 47:27–31. doi:10.1016/0020-7292(94)90457-X
Mesiano S, Chan EC, Fitter JT, Kwek K, Yeo G, Smith R (2002) Progesterone withdrawal and estrogen activation in human parturition are coordinated by progesterone receptor A expression in the myometrium. J Clin Endocrinol Metab 87:2924–2930. doi:10.1210/jc.87.6.2924
Fortson J, Howe L, Harmon C, Sherrill WW (2008) Targeting cardiovascular risk: early identification of insulin resistance. J Am Acad Nurse Pract 20:319–325. doi:10.1111/j.1745-7599.2008.00324.x
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Z. Ben-Zvi, G. Holcberg are equally contributed to this study.
Authors’ contributions: VF carried out the tissue processing, the perfusion experiments and wrote the manuscript. AA participated and advised throughout the perfusion experiments. BS was the connecting person with the delivery room and supplied the placentas. ES provided consultation regarding the statistical analysis and revised the manuscript. ZBZ and GH managed the project and revised the manuscript.
Rights and permissions
About this article
Cite this article
Feinshtein, V., Ben-Zvi, Z., Sheiner, E. et al. Progesterone levels in cesarean and normal delivered term placentas. Arch Gynecol Obstet 281, 387–392 (2010). https://doi.org/10.1007/s00404-009-1125-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-009-1125-x