Abstract
Purpose
Thyroid disorders are among the common endocrine problems in pregnant women. It is now well established that not only overt, but subclinical thyroid dysfunction also has adverse effects on maternal and fetal outcome. There are few data from India about the prevalence of thyroid dysfunction in pregnancy. With this background, this study aims to find prevalence of thyroid dysfunction in pregnancy and its impact on obstetrical outcome in Indian population.
Methods
Six hundred and 33 pregnant women in second trimester were registered. Detailed history and examination was done. Apart from routine obstetrical investigations, TSH level estimation was done. If TSH level was deranged then free T4 and thyroperoxidase antibody level estimation were done. Patients were managed accordingly and followed till delivery. Their obstetrical and perinatal outcomes were noted.
Results
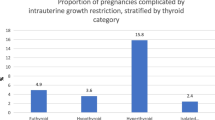
Prevalence of thyroid dysfunction was high in this study, with subclinical hypothyroidism in 6.47% and overt hypothyroidism in 4.58% women. Overt hypothyroids were prone to have pregnancy-induced hypertension (P = 0.04), intrauterine growth restriction (P = 0.01) and intrauterine demise (P = 0.0004) as compared to control. Cesarean section rate for fetal distress was significantly higher among pregnant subclinical hypothyroid women (P = 0.04). Neonatal complications and gestational diabetes were significantly more in overt hyperthyroidism group (P = 0.03 and P = 0.04, respectively).
Conclusions
Prevalence of thyroid disorders, especially overt and subclinical hypothyroidism (6.47%) was high. Significant adverse effects on maternal and fetal outcome were seen emphasizing the importance of routine antenatal thyroid screening.
Similar content being viewed by others

References
Casey BM, Dashe JS, Well CE et al (2005) Subclinical hypothyroidism and pregnancy outcomes. Obstet Gynecol 105:239–245
Vanderpump MPJ, Tunbridge WMG (2002) Epidemiology and prevention of clinical and subclinical hypothyroidism. Thyroid 12(10):839–846. doi:10.1089/105072502761016458
Poppe K, Glinoer D (2003) Thyroid autoimmunity and hypothyroidism before and during pregnancy. Hum Reprod Update 9(2):149–161. doi:10.1093/humupd/dmg012
Mestman J, Goodwin TM, Montoro MM (1995) Thyroid disorders of pregnancy. Endocrinol Metab Clin North Am 24:41–47
Leung AS, Millar LK, Koonings PP, Montoro M, Mestman J (1993) Perinatal outcomes in hypothyroid pregnancies. Obstet Gynecol 81(3):349–353
Mestman JH (1998) Hyperthyroidism in pregnancy. Endocrinol Metab Clin North Am 27(1):127–149. doi:10.1016/S0889-8529(05)70303-0
Miller LK, Wing DA, Leung AS, Koonings PP, Monotoro MN, Mestman JH (1994) Low birth weight and pre-eclampsia in pregnancies complicated by hyperthyroidism. Obstet Gynecol 84:946–949
Vaidya B, Anthony S, Bilous M et al (2007) Detection of thyroid dysfunction in early pregnancy: universal screening or targeted high risk case finding? J Clin Endocrinol Metab 92(1):203–207. doi:10.1210/jc.2006-1748
Wier FA, Farley CL (2006) Clinical controversies in screening women for thyroid disorders during pregnancy. J Midwifery Womens Health 51(3):152–158. doi:10.1016/j.jmwh.2005.11.007
Haddow JE, Palomaki GE, Allan WC et al (1999) Maternal thyroid deficiency during pregnancy and subsequent neuropsychological developments of the child. N Engl J Med 341:549–555. doi:10.1056/NEJM199908193410801
Rashid M, Rashid MH (2007) Obstetric management of thyroid disease. Obstet Gynecol Surv 62(10):680–688. doi:10.1097/01.ogx.0000281558.59184.b5 quiz 691
Lao TT (2005) Thyroid disorders in pregnancy. Curr Opin Obstet Gynecol 17:123–127. doi:10.1097/01.gco.0000162179.15360.08
Abalovich M, Gutierrez S, Alcarz G, Maccallini G, Garcia A, Levalle O (2002) Overt and subclinical hypothyroidism complicating pregnancy. Thyroid 12(1):63–67. doi:10.1089/105072502753451986
Smith C, Thomsett M, Choong C, Rodda Mclntyre HD, Cotterill AM (2001) Congenital thyrotoxicosis in premature infants. Horumon To Rinsho 54:371–376
Davis LE, Lucas MJ, Hankins GDV, Roark ML, Cunningham FG (1989) Thyrotoxicosis complicating pregnancy. Am J Obstet Gynecol 160:63–70
Abalovich M, Amino N, Barbour LA, Cobin RH, DeGroot LJ, Glinoer D, Mandel SJ, Stagnaro-Green A (2007) Management of thyroid dysfunction during pregnancy and postpartum: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 92(8)(Supp l):S1–S47. doi:10.1210/jc.2007-0141
Acknowledgments
We thank Human Resource Development Group, Council of Scientific and Industrial Research, New Delhi, India for financial aid.
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sahu, M.T., Das, V., Mittal, S. et al. Overt and subclinical thyroid dysfunction among Indian pregnant women and its effect on maternal and fetal outcome. Arch Gynecol Obstet 281, 215–220 (2010). https://doi.org/10.1007/s00404-009-1105-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-009-1105-1