Abstract
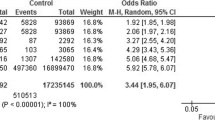
The relationship between acne vulgaris and oxidative stress biomarkers lacks a clear consensus. This study aimed to explore the potential correlation between acne vulgaris and circulating oxidative stress biomarkers (superoxide dismutase [SOD], malondialdehyde [MDA], and total antioxidant capacity [TAC]). We searched the PubMed, Embase, and Cochrane Library databases for articles published before June 26, 2023. The literature search combined free words and the medical subject headings terms related to acne vulgaris, SOD, MDA, and TAC. Data were analyzed using Stata 15 software. Additionally, we conducted a subgroup analysis stratified by the severity of acne vulgaris. A total of 14 trials involving 1191 participants were included. Overall results revealed that acne vulgaris was associated with MDA concentrations (SMD = 1.73; 95% CI 1.05, 2.4; P < 0.001). Subgroup analyses indicated that the severity of acne vulgaris was correlated with levels of circulating biomarkers of oxidative stress. TAC concentrations were significantly lower in patients with moderate acne vulgaris compared to controls (SMD = − 1.37; 95% CI = − 2.15, − 0.58, P = 0.001). SOD concentrations were significantly lower (SMD = − 2.92; 95% CI = − 5.39, − 0.46, P = 0.02) and MDA concentrations were significantly higher (SMD = 2.26; 95% CI = 0.95, 3.57, P = 0.001) in patients with severe acne vulgaris compared to controls. Our results implied that oxidative stress may exist in acne vulgaris. Furthermore, the severity of acne vulgaris was also correlated with oxidative stress.






Similar content being viewed by others
Data availability
Data will be made available on request.
Abbreviations
- CI:
-
Confidence interval
- MDA:
-
Malondialdehyde
- ROS:
-
Reactive oxygen species
- SMD:
-
Standard mean differences
- SOD:
-
Superoxide dismutase
- TAC:
-
Total antioxidant capacity
References
Eichenfield DZ, Sprague J, Eichenfield LF (2021) Management of acne vulgaris: a review. JAMA 326(20):2055–2067. https://doi.org/10.1001/jama.2021.17633
Lee YD, Yang JK, Han S, Kim BR, Shin JW, Bang J et al (2023) Topical methylene blue nanoformulation for the photodynamic therapy of acne vulgaris. Arch Dermatol Res 315(4):885–893. https://doi.org/10.1007/s00403-022-02464-7
Layton AM, Ravenscroft J (2023) Adolescent acne vulgaris: current and emerging treatments. Lancet Child Adolesc Health 7(2):136–144. https://doi.org/10.1016/S2352-4642(22)00314-5
Dawson AL, Dellavalle RP (2013) Acne vulgaris. BMJ (Clin Res Ed) 346:f2634. https://doi.org/10.1136/bmj.f2634
Habeshian KA, Cohen BA (2020) Current issues in the treatment of acne vulgaris. Pediatrics 145(Suppl 2):S225–S230. https://doi.org/10.1542/peds.2019-2056L
Sood S, Jafferany M, Vinaya KS (2020) Depression, psychiatric comorbidities, and psychosocial implications associated with acne vulgaris. J Cosmet Dermatol 19(12):3177–3182. https://doi.org/10.1111/jocd.13753
Zaenglein AL (2018) Acne vulgaris. N Engl J Med 379(14):1343–1352. https://doi.org/10.1056/NEJMcp1702493
Guler D, Soylu S, Guler HA (2023) The relationship of quality of life and acne severity with chronotype and insomnia in patients with acne vulgaris. Arch Dermatol Res 315(6):1689–1695. https://doi.org/10.1007/s00403-023-02569-7
Khan AQ, Agha MV, Sheikhan K, Younis SM, Tamimi MA, Alam M et al (2022) Targeting deregulated oxidative stress in skin inflammatory diseases: an update on clinical importance. Biomed Pharmacother 154:113601. https://doi.org/10.1016/j.biopha.2022.113601
Diao P, He H, Tang J, Xiong L, Li L (2021) Natural compounds protect the skin from airborne particulate matter by attenuating oxidative stress. Biomed Pharmacother. 138:111534. https://doi.org/10.1016/j.biopha.2021.111534
Guarneri F, Custurone P, Papaianni V, Gangemi S (2021) Involvement of RAGE and oxidative stress in inflammatory and infectious skin diseases. Antioxidants (Basel, Switzerland). 10(1):82. https://doi.org/10.3390/antiox10010082
Fibbi B, Marroncini G, Naldi L, Peri A (2023) The yin and yang effect of the apelinergic system in oxidative stress. Int J Mol Sci 24(5):4745. https://doi.org/10.3390/ijms24054745
Chang WL, Ko CH (2023) The role of oxidative stress in vitiligo: an update on its pathogenesis and therapeutic implications. Cells 12(6):936. https://doi.org/10.3390/cells12060936
Bickers DR, Athar M (2006) Oxidative stress in the pathogenesis of skin disease. J Invest Dermatol 126(12):2565–2575. https://doi.org/10.1038/sj.jid.5700340
Bungau AF, Radu AF, Bungau SG, Vesa CM, Tit DM, Endres LM (2023) Oxidative stress and metabolic syndrome in acne vulgaris: Pathogenetic connections and potential role of dietary supplements and phytochemicals. Biomed Pharmacother. 164:115003. https://doi.org/10.1016/j.biopha.2023.115003
Suh DH, Kwon HH (2015) What’s new in the physiopathology of acne? Br J Dermatol 172(Suppl 1):13–19. https://doi.org/10.1111/bjd.13634
Moradi Tuchayi S, Makrantonaki E, Ganceviciene R, Dessinioti C, Feldman SR, Zouboulis CC (2015) Acne vulgaris. Nat Rev Dis Primers 1:15029. https://doi.org/10.1038/nrdp.2015.29
Akamatsu H, Horio T, Hattori K (2003) Increased hydrogen peroxide generation by neutrophils from patients with acne inflammation. Int J Dermatol 42(5):366–369. https://doi.org/10.1046/j.1365-4362.2003.01540.x
Sarici G, Cinar S, Armutcu F, Altinyazar C, Koca R, Tekin NS (2010) Oxidative stress in acne vulgaris. J Eur Acad Dermatol Venereol JEADV 24(7):763–767. https://doi.org/10.1111/j.1468-3083.2009.03505.x
Abdel Fattah NS, Shaheen MA, Ebrahim AA, El Okda ES (2008) Tissue and blood superoxide dismutase activities and malondialdehyde levels in different clinical severities of acne vulgaris. Br J Dermatol 159(5):1086–1091. https://doi.org/10.1111/j.1365-2133.2008.08770.x
Arican O, Kurutas EB, Sasmaz S (2005) Oxidative stress in patients with acne vulgaris. Mediators Inflamm 2005(6):380–384. https://doi.org/10.1155/mi.2005.380
Dai S, Tian Z, Zhao D, Liang Y, Liu M, Liu Z et al (2022) Effects of coenzyme Q10 supplementation on biomarkers of oxidative stress in adults: a GRADE-assessed systematic review and updated meta-analysis of randomized controlled trials. Antioxidants (Basel, Switzerland). 11(7):1360. https://doi.org/10.3390/antiox11071360
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269. https://doi.org/10.7326/0003-4819-151-4-200908180-00135
Lo CK, Mertz D, Loeb M (2014) Newcastle–Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol 14:45. https://doi.org/10.1186/1471-2288-14-45
Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F et al (2015) The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med 8(1):2–10. https://doi.org/10.1111/jebm.12141
Higgins JP, Green S (2011). Cochrane handbook for systematic reviews of interventions (Version 5.1.0). The Cochrane Collaboration.
Hardy RJ, Thompson SG (1998) Detecting and describing heterogeneity in meta-analysis. Stat Med 17(8):841–856. https://doi.org/10.1002/(sici)1097-0258(19980430)17:8%3c841::aid-sim781%3e3.0.co;2-d
Takkouche B, Cadarso-Suarez C, Spiegelman D (1999) Evaluation of old and new tests of heterogeneity in epidemiologic meta-analysis. Am J Epidemiol 150(2):206–215. https://doi.org/10.1093/oxfordjournals.aje.a009981
Freedman BL, Danford CJ, Patwardhan V, Bonder A (2020) Treatment of overlap syndromes in autoimmune liver disease: a systematic review and meta-analysis. J Clin Med 9(5):1449. https://doi.org/10.3390/jcm9051449
Sisay M, Edessa D, Ali T, Mekuria AN, Gebrie A (2020) The relationship between advanced glycation end products and gestational diabetes: a systematic review and meta-analysis. PLoS ONE 15(10):e0240382. https://doi.org/10.1371/journal.pone.0240382
Doshi A, Zaheer A, Stiller MJ (1997) A comparison of current acne grading systems and proposal of a novel system. Int J Dermatol 36(6):416–418. https://doi.org/10.1046/j.1365-4362.1997.00099.x
Lehmann HP, Robinson KA, Andrews JS, Holloway V, Goodman SN (2002) Acne therapy: a methodologic review. J Am Acad Dermatol 47(2):231–240. https://doi.org/10.1067/mjd.2002.120912
Abdel Fattah NS, Ebrahim AA, El Okda ES (2011) Lipid peroxidation/antioxidant activity in patients with alopecia areata. J Eur Acad Dermatol Venereol JEADV 25(4):403–408. https://doi.org/10.1111/j.1468-3083.2010.03799.x
Abulnaja K (2009) Oxidant/antioxidant status in obese adolescent females with acne vulgaris. Indian J Dermatol 54(1):36–40. https://doi.org/10.4103/0019-5154.48984
Al-Shobaili HA (2014) Oxidants and anti-oxidants status in acne vulgaris patients with varying severity. Ann Clin Lab Sci 44(2):202–207
Awad SM, Morsy H, Sayed AA, Mohamed NA, Ezzat GM, Noaman MM (2018) Oxidative stress and psychiatric morbidity in patients with facial acne. J Cosmet Dermatol 17(2):203–208. https://doi.org/10.1111/jocd.12366
Basak PY, Gultekin F, Kilinc I (2001) The role of the antioxidative defense system in papulopustular acne. J Dermatol 28(3):123–127. https://doi.org/10.1111/j.1346-8138.2001.tb00105.x
Caliş B, Yerlikaya FH, Ataseven A, Temiz SA, Onmaz DE (2022) Oxidative stress-related miRNAs in patients with severe acne vulgaris. Indian J Dermatol 67(6):657–661. https://doi.org/10.4103/ijd.ijd_467_22
Demirkaya SK, Pektas SD, Küçükköse M, Ertuğrul Ö, Erel Ö (2016) Assessment of oxidative stress in adolescents with acne vulgaris and anxiety disorders. Biomed Res (India) 27(3):888–892
Ibrahim MA, Helmy ME, Sabry HH, Farouk SM, Ebrahim LY, Amer ER (2015) Evaluation of biomarkers of oxidant-antioxidant balance in patients with acne vulgaris. J Egypt Women’s Dermatol Soc 12(2):136–141. https://doi.org/10.1097/01.EWX.0000460812.60709.4e
Jisha R, SabooraBeegum M, Yogapriya V (2022) Oxidative stress in acne vulgaris. Int J Pharm Pharm Sci 14(11):73–76. https://doi.org/10.22159/ijpps.2022v14i11.45967
Moazen M, Mazloom Z, Jowkar F, Nasimi N, Moein Z, Vitamin D (2019) adiponectin, oxidative stress, lipid profile, and nutrient intakes in the females with acne vulgaris: a case–control study. Galen Med J 8:e1515. https://doi.org/10.31661/gmj.v8i0.1515
Yorulmaz Demir A, Metin A, Işikoǧlu S, Erel O (2012) The effect of isotretinoin on oxidative stress in severe acne vulgaris patients. Turk Klin J Med Sci 32(4):1026–1031. https://doi.org/10.5336/medsci.2011-26690
Popa GL, Mitran CI, Mitran MI, Tampa M, Matei C, Popa MI et al (2023) Markers of oxidative stress in patients with acne: a literature review. Life (Basel, Switzerland). 13(7):1433. https://doi.org/10.3390/life13071433
Zhang Y, Li Z, Ma Y, Mu Z (2019) Association of total oxidant status, total antioxidant status, and malondialdehyde and catalase levels with psoriasis: a systematic review and meta-analysis. Clin Rheumatol 38(10):2659–2671. https://doi.org/10.1007/s10067-019-04676-1
Speeckaert R, Dugardin J, Lambert J, Lapeere H, Verhaeghe E, Speeckaert MM et al (2018) Critical appraisal of the oxidative stress pathway in vitiligo: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol JEADV 32(7):1089–1098. https://doi.org/10.1111/jdv.14792
Huang TT, Zou Y, Corniola R (2012) Oxidative stress and adult neurogenesis—effects of radiation and superoxide dismutase deficiency. Semin Cell Dev Biol 23(7):738–744. https://doi.org/10.1016/j.semcdb.2012.04.003
Mohideen K, Chandrasekar K, Ramsridhar S, Rajkumar C, Ghosh S, Dhungel S (2023) Assessment of oxidative stress by the estimation of lipid peroxidation marker malondialdehyde (MDA) in patients with chronic periodontitis: a systematic review and meta-analysis. Int J Dent 2023:6014706. https://doi.org/10.1155/2023/6014706
Peluso I, Raguzzini A (2016) Salivary and urinary total antioxidant capacity as biomarkers of oxidative stress in humans. Patholog Res Int 2016:5480267. https://doi.org/10.1155/2016/5480267
Nobile V, Schiano I, Peral A, Giardina S, Sparta E, Caturla N (2021) Antioxidant and reduced skin-ageing effects of a polyphenol-enriched dietary supplement in response to air pollution: a randomized, double-blind, placebo-controlled study. Food Nutr Res 65. https://doi.org/10.29219/fnr.v65.5619
Burkhart CN, Burkhart CG (2003) Microbiology’s principle of biofilms as a major factor in the pathogenesis of acne vulgaris. Int J Dermatol 42(12):925–927. https://doi.org/10.1111/j.1365-4632.2003.01588.x
Agamia NF, El Mulla KF, Alsayed NM, Ghazala RM, El Maksoud REA, Abdelmeniem IM et al (2023) Isotretinoin treatment upregulates the expression of p53 in the skin and sebaceous glands of patients with acne vulgaris. Arch Dermatol Res 315(5):1355–1365. https://doi.org/10.1007/s00403-022-02508-y
Zouboulis CC (2004) Acne and sebaceous gland function. Clin Dermatol 22(5):360–366. https://doi.org/10.1016/j.clindermatol.2004.03.004
Ottaviani M, Alestas T, Flori E, Mastrofrancesco A, Zouboulis CC, Picardo M (2006) Peroxidated squalene induces the production of inflammatory mediators in HaCaT keratinocytes: a possible role in acne vulgaris. J Invest Dermatol 126(11):2430–2437. https://doi.org/10.1038/sj.jid.5700434
Akamatsu H, Horio T (1998) The possible role of reactive oxygen species generated by neutrophils in mediating acne inflammation. Dermatology (Basel, Switzerland) 196(1):82–85. https://doi.org/10.1159/000017876
ElAttar Y, Mourad B, Alngomy HA, Shams El Deen A, Ismail M (2022) Study of interleukin-1 beta expression in acne vulgaris and acne scars. J Cosmetic Dermatol. 21(10):4864–4870. https://doi.org/10.1111/jocd.14852
Fabbrocini G, Izzo R, Faggiano A, Del Prete M, Donnarumma M, Marasca C et al (2016) Low glycaemic diet and metformin therapy: a new approach in male subjects with acne resistant to common treatments. Clin Exp Dermatol 41(1):38–42. https://doi.org/10.1111/ced.12673
Kardeh S, Moein SA, Namazi MR, Kardeh B (2019) Evidence for the important role of oxidative stress in the pathogenesis of acne. Galen Med J 8:e1291. https://doi.org/10.31661/gmj.v0i0.1291
Kim JE, Han H, Xu Y, Lee MH, Lee HJ (2023) Efficacy of FRO on acne vulgaris pathogenesis. Pharmaceutics 15(7):1885. https://doi.org/10.3390/pharmaceutics15071885
Erturan İ, Naziroğlu M, Akkaya VB (2012) Isotretinoin treatment induces oxidative toxicity in blood of patients with acne vulgaris: a clinical pilot study. Cell Biochem Funct 30(7):552–557. https://doi.org/10.1002/cbf.2830
Fabbrocini G, Cameli N, Lorenzi S, De Padova MP, Marasca C, Izzo R et al (2014) A dietary supplement to reduce side effects of oral isotretinoin therapy in acne patients. Giornale Ital Dermatol Venereol 149(4):441–445
Chen H, Zhang TC, Yin XL, Man JY, Yang XR, Lu M (2022) Magnitude and temporal trend of acne vulgaris burden in 204 countries and territories from 1990 to 2019: an analysis from the Global Burden of Disease Study 2019. Br J Dermatol 186(4):673–683. https://doi.org/10.1111/bjd.20882
Cook-Bolden FE, Gold MH, Guenin E (2020) Tazarotene 0.045% lotion for the once-daily treatment of moderate-to-severe acne vulgaris in adult males. J Drugs Dermatol JDD. 19(1):78–85. https://doi.org/10.36849/JDD.2020.3979
Funding
This work was supported by the Yunnan Provincial Department of Education Science Research Fund Project (No. 2023Y0469), and Yunnan Provincial Clinical Medical Centre for Traditional Chinese Medicine Project (Dermatology).
Author information
Authors and Affiliations
Contributions
JY and XY: designed the review and provided methodological perspectives; LS and FW: performed the search, collected the data, analyzed the data, and wrote the manuscript; YW: wrote and reviewed the manuscript; CQ: reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interests
All authors report that there are no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Su, L., Wang, F., Wang, Y. et al. Circulating biomarkers of oxidative stress in people with acne vulgaris: a systematic review and meta-analysis. Arch Dermatol Res 316, 105 (2024). https://doi.org/10.1007/s00403-024-02840-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00403-024-02840-5