Abstract
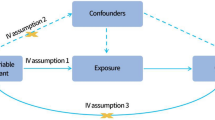
There have been reports of association between psoriasis and psychological illnesses. Nevertheless, it is not easy to draw conclusions with high quality causality from conventional observational studies. The objective of this study was to evaluate the causality of psoriasis and psychological illnesses. All summary-level data from genome-wide association studies for psoriasis and psychological illnesses were collected from Neale Lab and MRC Integrative Epidemiology Unit. Bidirectional Mendelian randomization analysis was performed to determine the random orientation with an independent genetic variation. The main estimated effects are derived using Inverse-Variance Weighted, weighted median, and MR Egger methods. Multiple data sets were validated against each other, and a series of sensitivity studies were conducted to ensure the reliability of the results. Mendelian randomization analysis revealed a causal effect of psoriasis [odds ratio (OR) 1·34, 95% confidence interval (CI) 1·21–1·46, P < 0.001; and OR 1.28, CI 1.17–1.39, P < 0.001] on psychological illnesses, and vice versa (OR 1.23, CI 1.14–1.31, P < 0.001; and OR 1.21, CI 1.11–1.31, P < 0.001). The results were supported by a series of sensitivity analyses. The findings of this Mendelian randomization study support a causal effect between psoriasis and psychological illnesses, and vice versa.


Similar content being viewed by others
Data availability
The data underlying this article were provided by IEU OpenGWAS by permission. All of the datasets are freely available from https://gwas.mrcieu.ac.uk/.
References
Rendon A, Schäkel K (2019) Psoriasis pathogenesis and treatment. Int J Mol Sci 20(6):1475. https://doi.org/10.3390/ijms20061475
Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker JNWN (2021) Psoriasis. The Lancet 397(10281):1301–1315. https://doi.org/10.1016/S0140-6736(20)32549-6
Kamiya K, Kishimoto M, Sugai J, Komine M, Ohtsuki M (2019) Risk factors for the development of psoriasis. Int J Mol Sci 20(18):E4347. https://doi.org/10.3390/ijms20184347
Takeshita J, Grewal S, Langan SM et al (2017) Psoriasis and comorbid diseases part II. implications for management. J Am Acad Dermatol 76(3):393–403. https://doi.org/10.1016/j.jaad.2016.07.065
Armstrong AW, Read C (2020) Pathophysiology, clinical presentation, and treatment of psoriasis: a review. JAMA 323(19):1945–1960. https://doi.org/10.1001/jama.2020.4006
Tohid H, Aleem D, Jackson C (2016) Major depression and psoriasis: a psychodermatological phenomenon. SPP 29(4):220–230. https://doi.org/10.1159/000448122
Bell KA, Balogh EA, Feldman SR (2021) An update on the impact of depression on the treatment of psoriasis. Expert Opin Pharmacother 22(6):695–703. https://doi.org/10.1080/14656566.2020.1849141
Amanat M, Salehi M, Rezaei N (2018) Neurological and psychiatric disorders in psoriasis. Rev Neurosci 29(7):805–813. https://doi.org/10.1515/revneuro-2017-0108
Pollo CF, Miot HA, de Matos TD et al (2021) Prevalence and factors associated with depression and anxiety in patients with psoriasis. J Clin Nurs 30(3–4):572–580. https://doi.org/10.1111/jocn.15577
Yu S, Tu HP, Huang YC, Lan CCE (2019) The incidence of anxiety may not be correlated with severity of psoriasis: a prospective pilot study. Med Hypotheses 130:109254. https://doi.org/10.1016/j.mehy.2019.109254
Matiushenko VP, Kutasevych YF, Havryliuk OA, Jafferany M (2020) Effectiveness of psychopharmacotherapy in psoriasis patients with associated anxiety and depression. Dermatol Ther 33(6):e14292. https://doi.org/10.1111/dth.14292
Levy I (2022) Stress, anxiety, and depression in times of COVID-19: Gender, individual quarantine, pandemic duration and employment. Front Public Health 10:999795. https://doi.org/10.3389/fpubh.2022.999795
Burgess S, Small DS, Thompson SG (2017) A review of instrumental variable estimators for Mendelian randomization. Stat Methods Med Res 26(5):2333–2355. https://doi.org/10.1177/0962280215597579
Wei J, Zhu J, Xu H et al (2022) Alcohol consumption and smoking in relation to psoriasis: a Mendelian randomization study. Br J Dermatol. https://doi.org/10.1111/bjd.21718
Freuer D, Linseisen J, Meisinger C (2022) Association between inflammatory bowel disease and both psoriasis and psoriatic arthritis: a bidirectional 2-sample Mendelian randomization study. JAMA Dermatol. https://doi.org/10.1001/jamadermatol.2022.3682
Gu X, Chen X, Shen M (2022) Association of psoriasis with risk of COVID-19: A 2-sample Mendelian randomization study. J Am Acad Dermatol 87(3):715–717. https://doi.org/10.1016/j.jaad.2022.01.048
Bowden J, Davey Smith G, Haycock PC, Burgess S (2016) Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol 40(4):304–314. https://doi.org/10.1002/gepi.21965
Burgess S, Thompson SG (2017) Interpreting findings from Mendelian randomization using the MR-Egger method. Eur J Epidemiol 32(5):377–389. https://doi.org/10.1007/s10654-017-0255-x
Kemp JP, Sayers A, Smith GD, Tobias JH, Evans DM (2016) Using Mendelian randomization to investigate a possible causal relationship between adiposity and increased bone mineral density at different skeletal sites in children. Int J Epidemiol 45(5):1560–1572. https://doi.org/10.1093/ije/dyw079
Cohen BE, Martires KJ, Ho RS (2016) Psoriasis and the risk of depression in the US population: national health and nutrition examination survey 2009–2012. JAMA Dermatol 152(1):73–79. https://doi.org/10.1001/jamadermatol.2015.3605
Egeberg A, Thyssen JP, Wu JJ, Skov L (2019) Risk of first-time and recurrent depression in patients with psoriasis: a population-based cohort study. Br J Dermatol 180(1):116–121. https://doi.org/10.1111/bjd.17208
Dalgard FJ, Gieler U, Tomas-Aragones L et al (2015) The psychological burden of skin diseases: a cross-sectional multicenter study among dermatological out-patients in 13 European countries. J Invest Dermatol 135(4):984–991. https://doi.org/10.1038/jid.2014.530
Min C, Kim M, Oh DJ, Choi HG (2020) Bidirectional association between psoriasis and depression: two longitudinal follow-up studies using a national sample cohort. J Affect Disord 262:126–132. https://doi.org/10.1016/j.jad.2019.10.043
Jalenques I, Bourlot F, Martinez E et al (2022) Prevalence and odds of anxiety disorders and anxiety symptoms in children and adults with psoriasis: systematic review and meta-analysis. Acta Derm Venereol 102:adv00769. https://doi.org/10.2340/actadv.v102.1386
Dowlatshahi EA, Wakkee M, Arends LR, Nijsten T (2014) The prevalence and odds of depressive symptoms and clinical depression in psoriasis patients: a systematic review and meta-analysis. J Invest Dermatol 134(6):1542–1551. https://doi.org/10.1038/jid.2013.508
Xiao Y, Zhang X, Luo D et al (2019) The efficacy of psychological interventions on psoriasis treatment: a systematic review and meta-analysis of randomized controlled trials. Psychol Res Behav Manag 12:97–106. https://doi.org/10.2147/PRBM.S195181
Esposito M, Saraceno R, Giunta A, Maccarone M, Chimenti S (2006) An Italian study on psoriasis and depression. Dermatology 212(2):123–127. https://doi.org/10.1159/000090652
Soliman MM (2021) Depressive, anxiety, stress, and insomnia symptoms in patients with psoriasis: a cross-sectional study. Postepy Dermatol Alergol 38(3):510–519. https://doi.org/10.5114/ada.2020.98726
Jing D, Xiao H, Shen M et al (2021) Association of psoriasis with anxiety and depression: a case-control study in chinese patients. Front Med (Lausanne) 8:771645. https://doi.org/10.3389/fmed.2021.771645
Bakar RS, Jaapar SZS, Azmi AF, Aun YC (2021) Depression and anxiety among patients with psoriasis: a correlation with quality of life and associated factors. J Taibah Univ Med Sci 16(4):491–496. https://doi.org/10.1016/j.jtumed.2021.02.008
Torales J, Echeverría C, Barrios I et al (2020) Psychodermatological mechanisms of psoriasis. Dermatol Ther 33(6):e13827. https://doi.org/10.1111/dth.13827
Zafiriou E, Daponte AI, Siokas V, Tsigalou C, Dardiotis E, Bogdanos DP (2021) Depression and obesity in patients with psoriasis and psoriatic arthritis: is IL-17-mediated immune dysregulation the connecting link? Front Immunol 12:699848. https://doi.org/10.3389/fimmu.2021.699848
Koo J, Marangell L, b., Nakamura M, et al (2017) Depression and suicidality in psoriasis: review of the literature including the cytokine theory of depression. J the Eur Acad Dermatol Venereol 31(12):1999–2009. https://doi.org/10.1111/jdv.14460
Wang X, Li Y, Wu L et al (2021) Dysregulation of the gut-brain-skin axis and key overlapping inflammatory and immune mechanisms of psoriasis and depression. Biomed Pharmacother 137:111065. https://doi.org/10.1016/j.biopha.2020.111065
Olejniczak-Staruch I, Ciążyńska M, Sobolewska-Sztychny D, Narbutt J, Skibińska M, Lesiak A (2021) Alterations of the skin and gut microbiome in psoriasis and psoriatic arthritis. Int J Mol Sci 22(8):3998. https://doi.org/10.3390/ijms22083998
Simpson CA, Diaz-Arteche C, Eliby D, Schwartz OS, Simmons JG, Cowan CSM (2021) The gut microbiota in anxiety and depression—a systematic review. Clin Psychol Rev 83:101943. https://doi.org/10.1016/j.cpr.2020.101943
Collins SM, Surette M, Bercik P (2012) The interplay between the intestinal microbiota and the brain. Nat Rev Microbiol 10(11):735–742. https://doi.org/10.1038/nrmicro2876
Davey Smith G, Holmes MV, Davies NM, Ebrahim S (2020) Mendel’s laws, Mendelian randomization and causal inference in observational data: substantive and nomenclatural issues. Eur J Epidemiol 35(2):99–111. https://doi.org/10.1007/s10654-020-00622-7
Acknowledgements
We thank the investigators of original genome-wide association study who provided the summary statistics.
Funding
This work was supported by a grant from the National Natural Science Foundation of China (NO.82074445).
Author information
Authors and Affiliations
Contributions
S. Liu and K. Yang designed the experimental protocol and wrote the main manuscript text. H. Zhang Performed database screening. Q. Yang and Y.Bai Provided expertise and guidance on key technologies. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare they have no conflicts of interest.
Ethical approval
The manuscript does not contain clinical studies or patient data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, S., Yang, K., Zhang, H. et al. The bidirectional causal association between psoriasis and psychological illnesses: a 2-sample Mendelian randomization study. Arch Dermatol Res 316, 40 (2024). https://doi.org/10.1007/s00403-023-02736-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00403-023-02736-w