Abstract
Importance
Hidradenitis suppurativa (HS) is associated with a number of physical and psychological comorbidities. Studies have suggested an association between HS and anemia; however, this association is not widely understood and may result in delayed diagnosis and treatment and possible increase in morbidity and mortality.
Objective
To systematically review and perform a meta-analysis regarding the association between HS and anemia, and to characterize the subtypes of anemia associated with HS.
Data sources
A search of the EMBASE, Medline, Web of Science Core Collection, and Cochrane Central Register of Controlled Trials databases from the time of database inception to September 25, 2022, yielded 313 unique articles.
Study selection
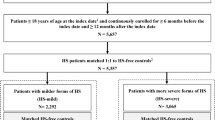
All observational studies and randomized controlled trials published in English that examined the odds ratio (OR) of anemia in patients with HS were screened by 2 independent reviewers. Case reports were excluded. Among 313 unique articles, 7 were deemed eligible.
Data extraction and synthesis
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines facilitated data extraction. The Newcastle–Ottawa Scale (NOS) was used to analyze risk of bias of included studies. In addition to OR and 95% confidence intervals, relevant data on patient demographics and anemia subtypes were also extracted.
Main outcomes and measures
The primary outcome was the OR of anemia in HS patients. This study also attempted to characterize anemia subtypes associated with HS.
Results
In total, 2 case–control and 5 cross-sectional studies featured a total of 11,693 patients. Among the studies, 4 of 7 demonstrated a statistically significant positive association between anemia and HS (ORs, 2.20 [1.42–3.41], 2.33 [1.99–2.73], 1.87 [1.02–3.44], and 1.50 [1.43–1.57]), with macrocytic and microcytic subtypes being most common. After adjusting for publication bias, meta-analysis with random effects revealed HS to be associated with increased odds of anemia compared to non-HS groups (OR 1.59 [1.19, 2.11]).
Conclusions and relevance
There is a statistically significant positive association between HS and anemia, particularly for the aforementioned subtypes. Patients with HS should be screened for anemia. In case of lower hemoglobin concentration, the anemia of HS patients should be subdivided according to mean corpuscular volume of the red blood cells and further investigated depending on subtype.



Similar content being viewed by others
Data availability
My manuscript has data as included in electronic supplementary material.
References
Alikhan A, Sayed C, Alavi A et al (2019) North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part I: diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol 81(1):76–90. https://doi.org/10.1016/j.jaad.2019.02.067
Nesbitt E, Clements S, Driscoll M (2019) A concise clinician’s guide to therapy for hidradenitis suppurativa. Int J Womens Dermatol 6(2):80–84. https://doi.org/10.1016/j.ijwd.2019.11.004
Revankar R, Murase J, Murrell D (2021) Shedding light on the impact of hidradentitis suppurativa on women and their families: a focus of the International Journal of Women’s Dermatology. Int J Womens Dermatol. https://doi.org/10.1016/j.ijwd.2021.08.005
Zouboulis CC, Desai N, Emtestam L et al (2015) European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa. J Eur Acad Dermatol Venereol 29(4):619–644. https://doi.org/10.1111/jdv.12966
Garg A, Wertenteil S, Baltz R et al (2018) Prevalence estimates for hidradenitis suppurativa among children and adolescents in the United States: a gender- and age- adjusted population analysis. J Invest Dermatol 138(10):2152–2156. https://doi.org/10.1016/j.jid.2018.04.001
Ingram JR, Jenkins-Jones S, Knipe DW et al (2018) Population-based Clinical Practice Research Datalink study using algorithm modelling to identify the true burden of hidradenitis suppurativa. Br J Dermatol. 178(4):917–924. https://doi.org/10.1111/bjd.16101
Jemec GB, Kimball AB (2015) Hidradenitis suppurativa: epidemiology and scope of the problem. J Am Acad Dermatol 73(5):S4–S7. https://doi.org/10.1016/j.jaad.2015.07.052
Bettoli V, Join-Lambert O, Nassif A (2016) Antibiotic treatment of hidradenitis suppurativa. Dermatol Clin 34(1):81–89. https://doi.org/10.1016/j.det.2015.08.013
Lee RA, Eisen DB (2015) Treatment of hidradenitis suppurativa with biologic medications. J Am Acad Dermatol 73(5 Suppl 1):S82–S88. https://doi.org/10.1016/j.jaad.2015.07.053
Melendez Gonzalez MDM, Sayed CJ (2020) Surgery is an essential aspect of managing patients with suppurativa. J Am Acad Dermatol 83(3):979–980. https://doi.org/10.1016/j.jaad.2020.03.008
Shah N (2005) Hidradenitis suppurativa: a treatment challenge. Am Fam Physician 72(8):1547–1552
van der Zee HH, Prens EP, Boer J (2010) Deroofing: a tissue-saving surgical technique for the treatment of mild to moderate hidradenitis suppurativa lesions. J Am Acad Dermatol 63(3):475–480. https://doi.org/10.1016/j.jaad.2009.12.018
Alavi A, Farzanfar D, Rogalska T et al (2018) Quality of life and sexual health in patients with hidradenitis suppurativa. Int J Womens Dermatol 4(2):74–79. https://doi.org/10.1016/j.ijwd.2017.10.007
Machado MO, Stergiopoulos V, Maes M et al (2019) Depression and anxiety in adults with hidradenitis suppurativa: a systematic review and meta-analysis. JAMA Dermatol 155(8):939–945. https://doi.org/10.1001/jamadermatol.2019.0759
Wright S, Strunk A, Garg A (2021) Prevalence of depression among children, adolescents, and adults with hidradenitis suppurativa. J Am Acad Dermatol S0190–9622(21):01947–01952. https://doi.org/10.1016/j.jaad.2021.06.843
Galán JL, Silvente C, González M et al (2020) Experience in patients with hidradenitis suppurativa and COVID-19 symptoms. J Am Acad Dermatol 83(4):e309–e311. https://doi.org/10.1016/j.jaad.2020.06.986
Price KN, Collier EK, Grogan TR, et al (2021) Hidradenitis suppurativa patient perspectives during the COVID-19 pandemic. Dermatol Online J 27(2):13030/qt42g0634s
Shah M, Naik HB, Alhusayen R (2020) Hidradenitis suppurativa: the importance of virtual outpatient care during COVID-19 pandemic. J Am Acad Dermatol 83(1):e81–e82. https://doi.org/10.1016/j.jaad.2020.04.142
Stout M (2020) The role of virtual support groups for patients with hidradenitis suppurativa during the COVID-19 pandemic. Int J Womens Dermatol 6(3):154–155. https://doi.org/10.1016/j.ijwd.2020.04.009
Cartron A, Driscoll MS (2019) Comorbidities of hidradenitis suppurativa: a review of the literature. Int J Womens Dermatol 5(5):330–334. https://doi.org/10.1016/j.ijwd.2019.06.026
Fimmel S, Zouboulis CC (2021) Comorbidities of hidradenitis suppurativa (acne inversa). Dermato-Endocrinol 2(1):9–16. https://doi.org/10.4161/derm.2.1.12490
Garg A, Malviya N, Strunk A et al (2021) Comorbidity screening in hidradenitis suppurativa: evidence-based recommendations from the US and Canadian Hidradenitis Suppurativa Foundations. J Am Acad Dermatol S0190–9622(21):00213–00219. https://doi.org/10.1016/j.jaad.2021.01.059
Tzellos T, Zouboulis CC (2020) Review of comorbidities of hidradenitis suppurativa: implications for daily clinical practice. Dermatol Ther (Heidelb) 10(1):63–71. https://doi.org/10.1007/s13555-020-00354-2
Cappellini MD, Motta I (2015) Anemia in clinical practice-definition and classification: does hemoglobin change with aging? Semin Hematol 52(4):261–269. https://doi.org/10.1053/j.seminhematol.2015.07.006
Le CH (2016) The Prevalence of Anemia and Moderate-Severe Anemia in the US Population (NHANES 2003–2012). PLoS One. 11(11):e0166635. https://doi.org/10.1371/journal.pone.0166635
Cascio MJ, DeLoughery TG (2017) Anemia: evaluation and diagnostic tests. Med Clin North Am 101(2):263–284. https://doi.org/10.1016/j.mcna.2016.09.003
Chaparro CM, Suchdev PS (2019) Anemia epidemiology, pathophysiology, and etiology in low- and middle-income countries. Ann N Y Acad Sci 1450(1):15–31. https://doi.org/10.1111/nyas.14092
Ghias M, Cameron S, Shaw F et al (2019) Anemia in hidradenitis suppurativa, hepcidin as a diagnostic tool. Am J Clin Path 152(1):15. https://doi.org/10.1093/ajcp/aqz112.029
Parameswaran A, Garshick M, Revankar R et al (2021) Hidradenitis suppurativa is associated with iron deficiency anemia, anemia of chronic disease, and sickle cell anemia—a single center retrospective cohort study. Int J Womens Dermatol. https://doi.org/10.1016/j.ijwd.2021.07.008
Kimball AB, Sundaram M, Gauthier G et al (2018) The comorbidity burden of hidradenitis suppurativa in the United States: a claims data analysis. Dermatol Ther (Heidelb) 8:557–569. https://doi.org/10.1007/s13555-018-0264-z
Narla S, Silverberg JI (2021) Autoimmune comorbidities of hidradenitis suppurativa in US adults and children. J Am Acad Dermatol. https://doi.org/10.1016/j.jaad.2019.06.129
Ponikowska M, Matusiak L, Kasztura M et al (2020) Deranged iron status evidenced by iron deficiency characterizes patients with hidradenitis suppurativa. Dermatology 236(1):52–58. https://doi.org/10.1159/000505184
Ramos-Rodriguez AJ, Timerman D, Khan A et al (2018) The in-hospital burden of hidradenitis suppurativa in patients with inflammatory bowel disease: a decade nationwide analysis from 2004 to 2014. Int J Dermatol 57(5):547–552. https://doi.org/10.1111/ijd.13932
Soliman YS, Chaitowitz M, Hoffman LK, Lin J, Lowes MA, Cohen SR (2020) Identifying anaemia in a cohort of patients with hidradenitis suppurativa. J Eur Acad Dermatol Venereol 34(1):e5–e8. https://doi.org/10.1111/jdv.15837
Miller IM, Johansen ME, Mogensen UB et al (2016) Is hidradenitis suppurativa associated with anaemia? A population-based and hospital-based cross-sectional study from Denmark. J Eur Acad Dermatol Venereol 30(8):1366–1372. https://doi.org/10.1111/jdv.13326
Shamseer L, Moher D, Clarke M, et al (2015) PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350:g7647. https://doi.org/10.1136/bmj.g7647
Lo CKL, Mertz D, Loeb M (2014) Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. https://doi.org/10.1186/1471-2288-14-45
Dowlatshahi EA, Wakkee M, Arends LR et al (2014) The prevalence and odds of depressive symptoms and clinical depression in psoriasis patients: a systematic review and meta-analysis. J Invest Dermatol 134(6):1542–1551. https://doi.org/10.1038/jid.2013.508
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Resnik SR, Geisler EL, Reyes N et al (2020) Prevalence and risk factors for anemia in a population with hidradenitis suppurativa. Cureus 12(12):e12015. https://doi.org/10.7759/cureus.12015
Phan K, Charlton O, Smith SD (2020) Global prevalence of hidradenitis suppurativa and geographical variation—systematic review and meta-analysis. Biomed Dermatol. https://doi.org/10.1186/s41702-019-0052-0
Seyed Jafari SM, Knüsel E, Cazzaniga S et al (2018) A retrospective cohort study on patients with hidradenitis suppurativa. Dermatology 234(1–2):71–78. https://doi.org/10.1159/000488344
Tun AM, Thein KZ, Myint ZW et al (2017) Pernicious anemia: fundamental and practical aspects in diagnosis. Cardiovasc Hematol Agents Med Chem 15(1):17–22. https://doi.org/10.2174/1871525715666170203114632
Chen WT, Chi CC (2019) Association of hidradenitis suppurativa with inflammatory bowel disease: a systematic review and meta-analysis. JAMA Dermatol 155(9):1022–1027. https://doi.org/10.1001/jamadermatol.2019.0891
Constantinou CA, Fragoulis GE, Nikiphorou E. Hidradenitis suppurativa: infection, autoimmunity, or both? Ther Adv Musculoskelet Dis. 2019;11:1759720X19895488. https://doi.org/10.1177/1759720X19895488
Cappellini MD, Comin-Colet J, de Francisco A, Dignass A, Doehner W, Lam CS, IRON CORE Group et al (2017) Iron deficiency across chronic inflammatory conditions: international expert opinion on definition, diagnosis, and management. Am J Hematol. 92(10):1068–78. https://doi.org/10.1002/ajh.24820
Jankowska EA, von Haehling S, Anker SD et al (2013) Iron deficiency and heart failure: diagnostic dilemmas and therapeutic perspectives. Eur Heart J 34(11):816–829. https://doi.org/10.1093/eurheartj/ehs224
Pagani A, Nai A, Silvestri L et al (2019) Hepcidin and anemia: a tight relationship. Front Physiol 10:1294. https://doi.org/10.3389/fphys.2019.01294
Hassell KL (2010) Population estimates of sickle cell disease in the U.S. Am J Prev Med 38:S512-21. https://doi.org/10.1016/j.amepre.2009.12.022
Kaitha S, Bashir M, Ali T (2015) Iron deficiency anemia in inflammatory bowel disease. World J Gastrointest Pathophysiol 6(3):62–72. https://doi.org/10.4291/wjgp.v6.i3
Funding
Authors did not received any funding for this work.
Author information
Authors and Affiliations
Contributions
AP and RR cultivated the ideas underlying the research question. AP, MR, SW, and RR performed the database search, data extraction, and methodological quality analysis. MR, RR, and HP performed the meta-analysis. MR, RR, HP, and NR prepared table and figures. AP, RR, HP, and JH wrote the manuscript. RR, NR and JH prepared the submission materials. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Senior author: Anupama Parameswaran.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Revankar, R., Rojas, M., Walsh, S. et al. Anemia in patients with hidradenitis suppurativa. Arch Dermatol Res 315, 1639–1648 (2023). https://doi.org/10.1007/s00403-023-02559-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-023-02559-9