Abstract
Introduction
Little is known regarding characteristics of hospitalized dermatomyositis (DM) patients. Understanding the unique characteristics of hospitalized DM patients with underlying malignancy is important in guiding development of specific work-up and treatment algorithms.
Objectives
We aim to characterize the inpatient burden of DM patients with malignancy (DM malignancy), determine unique characteristics of DM-malignancy inpatients, and assess trends and predictors of cost of care and length of stay for hospitalized DM-malignancy patients.
Methods
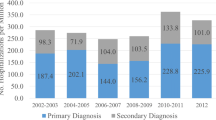
Hospitalized DM patients with and without malignancy were characterized and compared using 2009–2015 National Inpatient Sample. Associated malignancies, risk factors for malignancy, and trends/predictors for cost of care and length of stay were evaluated using multivariable models.
Results
Prevalence of malignancies among hospitalized DM inpatients was 10.9%. Age > 40 years and female sex were significantly associated with increased malignancy risk in DM inpatients. Numerous malignancies were significantly more common in men with DM compared to women, including bronchial, non-Hodgkin’s lymphoma, head/neck, bladder, esophageal, kidney, and stomach. The most common malignancies in women with DM were breast and ovarian. Head/neck carcinomas were more common in hospitalized DM patients than previous cohorts evaluating outpatients. Socioeconomic characteristics differed between DM patients with/without malignancy. The presence of underlying malignancy did not affect hospitalization cost, length of stay, or mortality in the hospitalized DM population. The economic burden of hospitalized DM patients is increasing over time.
Conclusions
DM inpatients with malignancy display numerous differences compared to DM inpatients without malignancy. Further research characterizing hospitalized DM patients is warranted in order to optimize work-up and treatment guidelines for these patients.

Similar content being viewed by others
Availability of data and material
Publicly accessible through the Healthcare Cost and Utilization Project.
References
Stertz G (1916) Polymyositis. Berl Klin Wochenschr 53(489):241–266
Lu X, Yang H, Shu X et al (2014) Factors predicting malignancy in patients with polymyositis and dermatomyostis: a systematic review and meta-analysis. Kuwana M, ed. PLoS ONE 9(4):e94128. https://doi.org/10.1371/journal.pone.0094128
Risk of Cancer in Dermatomyositis or Polymyositis (1992) N Engl J Med 327(3):207–208. https://doi.org/10.1056/NEJM199207163270318
Hill CL, Zhang Y, Sigurgeirsson B et al (2001) Frequency of specific cancer types in dermatomyositis and polymyositis: a population-based study. Lancet 357(9250):96–100. https://doi.org/10.1016/S0140-6736(00)03540-6
Yang Z, Lin F, Qin B, Liang Y, Zhong R (2015) Polymyositis/Dermatomyositis and Malignancy Risk: A Metaanalysis Study. J Rheumatol 42:282–291. https://doi.org/10.3899/jrheum.140566
Olazagasti JM, Baez PJ, Wetter DA, Ernste FC (2015) Cancer risk in dermatomyositis: a meta-analysis of cohort studies. Am J Clin Dermatol 16(2):89–98. https://doi.org/10.1007/s40257-015-0120-1
Healthcare Cost and Utilization Project (HCUP) HCUP National Inpatient Sample (NIS). Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 1 Aug 2018
National Center for Health Statistics (NCHS) (2013) ICD-9-CM: International Classification of Diseases, Ninth Revision, Clinical Modification. Baltimore, MD: U.S. National Library of Medicine; 2013. https://www.nlm.nih.gov/research/umls/sourcereleasedocs/current/ICD9CM/metadata.html. Accessed 1 Aug 2018
Kwa MC, Ardalan K, Laumann AE, Nardone B, West DP, Silverberg JI (2017) Validation of international classification of diseases codes for the epidemiologic study of dermatomyositis. Arthritis Care Res (Hoboken) 69(5):753–757. https://doi.org/10.1002/acr.23010
Silverberg JI, Kwa L, Kwa MC, Laumann AE, Ardalan K (2018) Cardiovascular and cerebrovascular comorbidities of juvenile dermatomyositis in US children: an analysis of the National Inpatient Sample. Rheumatology 57(4):694–702. https://doi.org/10.1093/rheumatology/kex465
Wei W-Q, Bastarache LA, Carroll RJ et al (2017) Evaluating phecodes, clinical classification software, and ICD-9-CM codes for phenome-wide association studies in the electronic health record. Rzhetsky A. ed. PLoS ONE 12(7):e0175508. https://doi.org/10.1371/journal.pone.0175508
HCUP (2016) Appendix A: Clinical Classification Software-Diagnoses. AHRQ. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/AppendixASingleDX.txt. Published 2016. Accessed 24 March 2016
Healthcare Cost and Utilization Project (2018) HCUP-US Tools and Software Page CCS-Services and Procedures. AHRQ. https://www.hcup-us.ahrq.gov/toolssoftware/ccs_svcsproc/ccssvcproc.jsp#details. Published 2015. Accessed 3 Oct 2018
Bureau of Labor Statistics. Consumer Price Index Inflation Calculator. Databases, Tables, and Calculators. https://www.bls.gov/data/inflation_calculator.htm.
Hsu DY, Shinkai K, Silverberg JI (2018) Epidemiology of eczema herpeticum in hospitalized U.S. children: analysis of a nationwide cohort. J Invest Dermatol. 138(2):265–272. https://doi.org/10.1016/j.jid.2017.08.039
Di Rollo D, Abeni D, Tracanna M, Capo A, Amerio P (2014) Cancer risk in dermatomyositis: a systematic review of the literature. G Ital Dermatol Venereol. 149(5):525–537. https://www.ncbi.nlm.nih.gov/pubmed/24975953. Accessed 25 July 2018
Chapireau D, Adlam D, Cameron M, Thompson M (2010) Paraneoplastic syndromes in patients with primary oral cancers: a systematic review. Br J Oral Maxillofac Surg 48(5):338–344. https://doi.org/10.1016/j.bjoms.2009.08.025
Fardet L, Dupuy A, Gain M et al (2009) Factors associated with underlying malignancy in a retrospective cohort of 121 patients with dermatomyositis. Medicine (Baltimore) 88(2):91–97. https://doi.org/10.1097/MD.0b013e31819da352
Botsios C, Ostuni P, Boscolo-Rizzo P, Da Mosto MC, Punzi L, Marchiori C (2003) Dermatomyositis and malignancy of the pharynx in Caucasian patients: report of two observations. Rheumatol Int 23(6):309–311. https://doi.org/10.1007/s00296-003-0319-y
Buchbinder R, Forbes A, Hall S, Dennett X, Giles G (2001) Incidence of malignant disease in biopsy-proven inflammatory myopathy. A population-based cohort study. Ann Intern Med 134(12):1087–1095. https://www.ncbi.nlm.nih.gov/pubmed/11412048. Accessed 30 Jan 2019
Ling DC, Kabolizadeh P, Heron DE et al (2015) Incidence of hospitalization in patients with head and neck cancer treated with intensity-modulated radiation therapy. Head Neck 37(12):1750–1755. https://doi.org/10.1002/hed.23821
Kang H-S, Roh J-L, Lee S-W et al (2016) Noncancer-Related Health Events and Mortality in Head and Neck Cancer Patients After Definitive Radiotherapy: A Prospective Study. Medicine (Baltimore) 95(19):e3403. https://doi.org/10.1097/MD.0000000000003403
Kwon M, Roh J-L, Song J et al (2014) Noncancer health events as a leading cause of competing mortality in advanced head and neck cancer. Ann Oncol 25(6):1208–1214. https://doi.org/10.1093/annonc/mdu128
Adi AH, Alturkmani H, Spock T et al (2015) Dermatomyositis paraneoplastic syndrome before symptomatic tonsillar squamous cell carcinoma: A case report. Anderson P, ed. Head Neck 37(1):E1–E3. https://doi.org/10.1002/hed.23703
Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA (2000) Gender differences in the utilization of health care services. J Fam Pract 49(2):147–152
Shen S, Wolfe R, McLean CA, Haskett M, Kelly JW (2014) Characteristics and associations of high-mitotic-rate melanoma. JAMA Dermatol 150(10):1048. https://doi.org/10.1001/jamadermatol.2014.635
Nosrati A, Wei ML (2014) Sex disparities in melanoma outcomes: the role of biology, vol 563. Academic Press Inc., Cambridge, pp 42–50 https://doi.org/10.1016/j.abb.2014.06.018
Gamba CS, Clarke CA, Keegan THM, Tao L, Swetter SM (2013) Melanoma survival disadvantage in young, non-hispanic white males compared with females. JAMA Dermatol 149(8):912. https://doi.org/10.1001/jamadermatol.2013.4408
Chow W-H, Gridley G, Mellemkjær L, McLaughlin JK, Olsen JH, Fraumeni JF (1995) Cancer risk following polymyositis and dermatomyositis: a nationwide cohort study in Denmark. Cancer Causes Control 6(1):9–13. https://doi.org/10.1007/BF00051675
Bendewald MJ, Wetter DA, Li X, Davis MDP (2010) Incidence of dermatomyositis and clinically amyopathic dermatomyositis. Arch Dermatol 146(1):26–30. https://doi.org/10.1001/archdermatol.2009.328
Kooistra L, Ricotti C, Galimberti F, Gota C, Fernandez AP (2018) Malignancy-associated dermatomyositis: retrospective case–control study from a single tertiary care center. J Am Acad Dermatol 79(1):152–155. https://doi.org/10.1016/j.jaad.2018.01.002
Hsu D, Brieva J, Silverberg JI (2016) Costs of care for hospitalization for pemphigus in the United States. JAMA Dermatology 152(6):645. https://doi.org/10.1001/jamadermatol.2015.5240
Sammon JD, McKay RR, Kim SP et al (2015) Burden of hospital admissions and utilization of hospice care in metastatic prostate cancer patients. Urology 85(2):343–350. https://doi.org/10.1016/j.urology.2014.09.053
Gourin CG, Frick KD (2012) National trends in oropharyngeal cancer surgery and the effect of surgeon and hospital volume on short-term outcomes and cost of care. Laryngoscope 122(3):543–551. https://doi.org/10.1002/lary.22447
Kono H, Inokuma S, Nakayama H, Suzuki M (2000) Pneumomediastinum in dermatomyositis: association with cutaneous vasculopathy. Ann Rheum Dis 59(5):372–376. https://www.ncbi.nlm.nih.gov/pubmed/10784520. Accessed 26 July 2018
Waldman R, DeWane ME, Lu J (2020) Dermatomyositis: diagnosis and treatment. J Am Acad Dermatol 82(2):283–296. https://doi.org/10.1016/j.jaad.2019.05.105
Trallero-Araguás E, Rodrigo-Pendás JÁ, Selva-O’Callaghan A et al (2012) Usefulness of anti-p155 autoantibody for diagnosing cancer-associated dermatomyositis: A systematic review and meta-analysis. Arthritis Rheum 64(2):523–532. https://doi.org/10.1002/art.33379
Best M, Molinari N, Chasset F, Vincent T, Cordel N, Bessis D (2019) Use of anti-transcriptional intermediary factor-1 gamma autoantibody in identifying adult dermatomyositis patients with cancer: a systematic review and meta-analysis. Acta Derm Venereol 99(3):256–262. https://doi.org/10.2340/00015555-3091
Fiorentino DF, Chung LS, Christopher-Stine L et al (2013) Most patients with cancer-associated dermatomyositis have antibodies to nuclear matrix protein NXP-2 or transcription intermediary factor 1γ. Arthritis Rheum 65(11):2954–2962. https://doi.org/10.1002/art.38093
Yang H, Peng Q, Yin L et al (2017) Identification of multiple cancer-associated myositis-specific autoantibodies in idiopathic inflammatory myopathies: a large longitudinal cohort study. Arthritis Res Ther. https://doi.org/10.1186/s13075-017-1469-8
Lim CH, Tseng C-W, Lin C-T et al (2018) The clinical application of tumor markers in the screening of malignancies and interstitial lung disease of dermatomyositis/polymyositis patients: a retrospective study. SAGE Open Med 6:205031211878189. https://doi.org/10.1177/2050312118781895
Selva-O’Callaghan A, Martinez-Gómez X, Trallero-Araguás E, Pinal-Fernández I (2018) The diagnostic work-up of cancer-associated myositis. Curr Opin Rheumatol. 30(6):630–636. https://doi.org/10.1097/BOR.0000000000000535
Acknowledgments
We would like to acknowledge the Medicine, Society, and Culture program in the Department of Bioethics at Case Western Reserve University School of Medicine for supporting our access to this database.
Funding
There is no financial support for this study.
Author information
Authors and Affiliations
Contributions
RT had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: RT, APF. Acquisition, analysis, and interpretation of data: RT. Drafting of the manuscript: RT, APF. Critical revision of the manuscript for important intellectual content: RT, APF. Statistical analysis: RT. Administrative, technical, or material support: RT, APF. Study supervision: RT, APF.
Corresponding author
Ethics declarations
Conflicts of Interest
A.P.F. is an investigator for Pfizer, Corbus, Mallinckrodt, and Novartis pharmaceuticals. He receives personal research support from Mallinckrodt and Novartis; honorarium from AbbVie, UCB, Novartis, and Mallinckrodt for consulting and advisory board participation, and honorarium from AbbVie, Novartis and Mallinckrodt for teaching and speaking. R.T. reports no conflicts of interest.
Code availability
By request.
Ethics approval
IRB approval was not necessary for use of this publicly available, de-identified database.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tripathi, R., Fernandez, A.P. Characteristics of hospitalized dermatomyositis patients with underlying malignancy: a nationally representative retrospective cohort study. Arch Dermatol Res 313, 473–482 (2021). https://doi.org/10.1007/s00403-020-02127-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-020-02127-5