Abstract
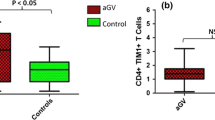
Several studies demonstrated a major pathological role of melanocyte-specific cytotoxic CD8+ T cells in the pathogenesis of vitiligo. It has been suggested that apoptosis, rather than necrosis, is the mechanism of melanocyte depletion in vitiligo. The aim of this study was to evaluate the expression and distribution of perforin and apoptosis stimulation fragment ligand (FasL) in the epidermis and dermis of the perilesional and non-lesional skin of vitiligo patients in comparison to controls, to assess their possible role in mediating apoptosis in vitiligo. Twenty patients with active non-segmental vitiligo and 20 healthy controls were enrolled in the study. Skin biopsies were taken from perilesional and non-lesional skin of patients with vitiligo, as well as covered skin of controls. Immunostaining for perforin and FasL was performed and the quantitative analysis for the expression of perforin and FasL was carried out in the epidermis and dermis of biopsied specimens. Epidermal perforin, dermal perforin, epidermal FasL, dermal FasL were significantly higher in perilesional as well as non-lesional skin than controls. There was a statistically significant positive correlation between epidermal and dermal perforin in perilesional skin. There was a statistically significant positive correlation between epidermal and dermal perforin, as well as epidermal and dermal FasL in non-lesional skin. In conclusion, the significant expression of perforin and FasL in the epidermis and dermis of both perilesional and non-lesional skin of active vitiligo patients suggests the role of cytotoxic granules and apoptotic cell death pathways in the pathogenesis of active vitiligo.




Similar content being viewed by others
References
Benzekri L, Gauthier Y (2017) Clinical markers of vitiligo activity. J Am Acad Dermatol 76:856–862
Bishnoi A, Parsad D (2018) Clinical and molecular aspects of vitiligo treatments. Int J Mol Sci 19(5):1509
Cheuk S, Schlums H, Gallais Sérézal I, Martini E, Chiang SC, Marquardt N, Gibbs A, Detlofsson E, Introini A, Forkel M, Höög C, Tjernlund A, Michaëlsson J, Folkersen L, Mjösberg J, Blomqvist L, Ehrström M, Ståhle M, Bryceson YT, Eidsmo L (2017) CD49a expression defines tissue-resident CD8+ T cells poised for cytotoxic function in human skin. Immunity 46(2):287–300
Hamzavi I, Jain H, McLean D, Shapiro J, Zeng H, Lui H (2004) Parametric modeling of narrowband UV-B phototherapy for vitiligo using a novel quantitative tool: the Vitiligo Area Scoring Index. Arch Dermatol 140(6):677–683
Huang CL, Nordlund JJ, Boissy R (2002) Vitiligo: a manifestation of apoptosis? Am J Clin Dermatol 3(5):301–308
Lambe T, Leung JC, Bouriez-Jones T, Silver K, Makinen K, Crockford TL, Ferry H, Forrester JV, Cornall RJ (2006) CD4 T lymphocytes-dependent autoimmunity against a melanocyte neoantigen induces spontaneous vitiligo and depends upon Fas-Fas ligand interactions. J Immunol 177:3055–3062
Lang KS, Caroli CC, Muhm A, Wernet D, Moris A, Schittek B, Knauss-Scherwitz E, Stevanovic S, Rammensee HG, Garbe C (2001) HLA-A2 restricted, melanocyte-specific CD8(+) T lymphocytes detected in vitiligo patients are related to disease activity and are predominantly directed against MelanA/MART1. J Invest Dermatol 116:891–897
Le Gal FA, Avril MF, Bosq J, Lefebvre P, Deschemin JC, Andrieu M, Knauss-Scherwitz E, Stevanovic S, Rammensee HG, Garbe C (2001) Direct evidence to support the role of antigen-specific CD8(+) T cells in melanoma-associated vitiligo. J Invest Dermatol 117:1464–1470
Le Poole IC, van den Wijngaard RM, Westerhof W, Das PK (1996) Presence of T cells and macrophages in inflammatory vitiligo skin parallels melanocyte disappearance. Am J Pathol 148(4):1219–1228
Li M, Sun D, Li C, Zhang Z, Gao L, Li K, Li H, Gao T (2008) Functional polymorphisms of the FAS gene associated with risk of vitiligo in Chinese populations: a case-control analysis. J Invest Dermatol 128:2820–2824
Lopez JA, Susanto O, Jenkins MR, Lukoyanova N, Sutton VR, Law RH, Johnston A, Bird CH, Bird PI, Whisstock JC, Trapani JA, Saibil HR, Voskoboinik I (2013) Perforin forms transient pores on the target cell plasma membrane to facilitate rapid access of granzymes during killer cell attack. Blood 121:2659–2668
Nabhani S, Ginzel S, Miskin H, Revel-Vilk S, Harlev D, Fleckenstein B, Hönscheid A, Oommen PT, Kuhlen M, Thiele R, Laws HJ, Borkhardt A, Stepensky P, Fischer U (2015) Deregulation of Fas ligand expression as a novel cause of autoimmune lymphoproliferative syndrome-like disease. Haematologica 100(9):1189–1198
Njoo MD, Das PK, Bos JD, Westerhof W (1999) Association of the Köbner phenomenon with disease activity and therapeutic responsiveness in vitiligo vulgaris. Arch Dermatol 135(4):407–413
Ongenae K, Van Geel N, Naeyaert JM (2003) Evidence for an autoimmune pathogenesis of vitiligo. Pigment Cell Res 16:90–100
Pretti Aslanian FM, Noé RA, Antelo DP, Farias RE, Das PK, Galadari I, Cuzzi T, Filgueira AL (2008) Immunohistochemical findings in active vitiligo including depigmenting lesions and non-lesional skin. Open Dermatol J 2:105–110
Pretti Aslanian FM, Noe RA, Cuzzi T, Filgueira AL (2007) Abnormal histological findings in active vitiligo include the normal-appearing skin. Pigment Cell Res 20(2):144–145
Saleh FY, Awad SS, Sadek IM (2013) Lymphocytic expression of Fas and FasL apoptotic markers in vitiligo. Clin Med Res 2:105–109
Su SC, Chung WH (2014) Cytotoxic proteins and therapeutic targets in severe cutaneous adverse reactions. Toxins (Basel) 6(1):194–210
Sweet RD (1978) Vitiligo as a Koebner phenomenon. Br J Dermatol 99:223–224
van den Boorn JG, Konijnenberg D, Dellemijn TA, van der Veen JP, Bos JD, Melief CJ, Vyth-Dreese FA, Luiten RM (2009) Autoimmune destruction of skin melanocytes by perilesional T cells from vitiligo patients. J Invest Dermatol 129:2220–2232
van den Wijngaard R, Wankowicz-Kalinska A, Le Poole C, Tigges B, Westerhof W, Das P (2000) Local immune response in skin of generalized vitiligo patients Destruction of melanocytes is associated with the prominent presence of CLA+ T cells at the perilesional site. Lab Invest 80(8):1299–1309
Wehrli P, Viard I, Bullani R, Tschopp J, French LE (2000) Death receptors in cutaneous biology and disease. J Invest Dermatol 115(2):141–148
Wu J, Zhou M, Wan Y, Xu A (2013) CD8+ T cells from vitiligo perilesional margins induce autologous melanocyte apoptosis. Mol Med Rep 7(1):237–241
Yang Y, Li S, Zhu G, Zhang Q, Wang G, Gao T, Li C, Wang L, Jian Z (2017) A similar local immune and oxidative stress phenotype in vitiligo and halo nevus. J Dermatol Sci 87(1):50–59
You S, Cho Y, Byun JS, Shin EC (2013) Melanocyte-specific CD8+ T cells are associated with epidermal depigmentation in a novel mouse model of vitiligo. Clin Exp Immunol 174(1):38–44
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hassan, A.S., Kohil, M.M., Sayed, S.S.E. et al. Immunohistochemical study of perforin and apoptosis stimulation fragment ligand (FasL)in active vitiligo. Arch Dermatol Res 313, 453–460 (2021). https://doi.org/10.1007/s00403-020-02117-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-020-02117-7