Abstract
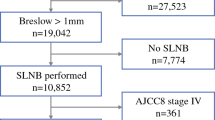
Factors that are most associated with positive lymph node status in melanoma are Breslow thickness and ulceration. However, there are other factors that have been little explored and could help in the identification of “at risk patients” harbouring occult metastasis. The objective of this study was to determine whether intensity of tumour-infiltrating lymphocytes (TILs) in a cohort study (N = 4133) is an independent predictor of sentinel lymph node (SLN) status in patients with primary cutaneous melanoma. Of the patients with cutaneous melanoma who resulted negative for nodal metastasis, 50.7% had moderate/marked TILs versus 27.7% among those patients who resulted positive for nodal metastasis. In the multivariate analysis, controlling for sex, age, mitotic rate, ulceration and Breslow, high levels of TILs in primary invasive melanoma was associated with a lower risk of developing SLN metastasis (OR 0.46; 95% CI 0.23–0.95, p = 0.037). When the analysis was stratified by sex, the protective effect of moderate/marked TIL remained only for women (OR 0.30; 95% CI 0.10–0.93, p = 0.037) but not for men (OR 0.51; 95% CI 0.19–1.34, p = 0.172). Other independent predictors of negative lymph node were low Breslow thickness (≤ 2.0 mm) and low mitotic rate. Besides predicting a negative lymph node response, TILs were also associated with a decreased risk of 10-year mortality among females with positive lymph node. Our findings suggest that high level of TILs is an independent predictor of negative SLN status among women. Further research is warranted to confirm our findings.
Similar content being viewed by others
References
Azimi F, Scolyer RA, Rumcheva P, Moncrieff M, Murali R, McCarthy SW, Saw RP, Thompson JF (2012) Tumor-infiltrating lymphocyte grade is an independent predictor of sentinel lymph node status and survival in patients with cutaneous melanoma. J Clin Oncol 30:2678–2683. https://doi.org/10.1200/jco.2011.37.8539
Barnhill R (1995) Pathology of melanocytic nevi and malignant melanoma. Butterworth-Heinemann, Boston
Breslow A (1970) Thickness, cross-sectional areas and depth of invasion in the prognosis of cutaneous melanoma. Ann Surg 172:902–908
Burton AL, Roach BA, Mays MP, Chen AF, Ginter BA, Vierling AM, Scoggins CR, Martin RC, Stromberg AJ, Hagendoorn L, McMasters KM (2011) Prognostic significance of tumor infiltrating lymphocytes in melanoma. Am Surg 77:188–192
Caggiati A, Potenza C, Gabrielli F, Passarelli F, Tartaglione G (2000) Sentinel node biopsy for malignant melanoma: analysis of a 4-year experience. Tumori 86:332–335
Chang JM, Kosiorek HE, Dueck AC, Leong SPL, Vetto JT, White RL, Avisar E, Sondak VK, Messina JL, Zager JS, Garberoglio C, Kashani-Sabet M, Pockaj BA (2018) Stratifying SLN incidence in intermediate thickness melanoma patients. Am J Surg 215:699–706. https://doi.org/10.1016/j.amjsurg.2017.12.009
Conic RRZ, Ko J, Damiani G, Funchain P, Knackstedt T, Vij A, Vidimos A, Gastman BR (2019) Predictors of sentinel lymph node positivity in thin melanoma using the National Cancer Database. J Am Acad Dermatol 80:441–447
Dronca RS, Dong H (2015) A gender factor in shaping T-cell immunity to melanoma. Front Oncol 5:8. https://doi.org/10.3389/fonc.2015.00008
Faries MB, Thompson JF, Cochran AJ, Andtbacka RH, Mozzillo N, Zager JS, Jahkola T, Bowles TL, Testori A, Beitsch PD, Hoekstra HJ, Moncrieff M, Ingvar C, Wouters M, Sabel MS, Levine EA, Agnese D, Henderson M, Dummer R, Rossi CR, Neves RI, Trocha SD, Wright F, Byrd DR, Matter M, Hsueh E, MacKenzie-Ross A, Johnson DB, Terheyden P, Berger AC, Huston TL, Wayne JD, Smithers BM, Neuman HB, Schneebaum S, Gershenwald JE, Ariyan CE, Desai DC, Jacobs L, McMasters KM, Gesierich A, Hersey P, Bines SD, Kane JM, Barth RJ, McKinnon G, Farma JM, Schultz E, Vidal-Sicart S, Hoefer RA, Lewis JM, Scheri R, Kelley MC, Nieweg OE, Noyes RD, Hoon DSB, Wang HJ, Elashoff DA, Elashoff RM (2017) Completion dissection or observation for sentinel-node metastasis in melanoma. N Engl J Med 376:2211–2222. https://doi.org/10.1056/NEJMoa1613210
Fortes C, Mastroeni S, Mannooranparampil TJ, Passarelli F, Zappala A, Annessi G, Marino C, Caggiati A, Russo N, Michelozzi P (2015) Tumor-infiltrating lymphocytes predict cutaneous melanoma survival. Melanoma Res 25:306–311. https://doi.org/10.1097/cmr.0000000000000164
Han D, Zager JS, Shyr Y, Chen H, Berry LD, Iyengar S, Djulbegovic M, Weber JL, Marzban SS, Sondak VK, Messina JL, Vetto JT, White RL, Pockaj B, Mozzillo N, Charney KJ, Avisar E, Krouse R, Kashani-Sabet M, Leong SP (2013) Clinicopathologic predictors of sentinel lymph node metastasis in thin melanoma. J Clin Oncol 31:4387–4393. https://doi.org/10.1200/jco.2013.50.1114
Hanna AN, Sinnamon AJ, Roses RE, Kelz RR, Elder DE, Xu X, Pockaj BA, Zager JS, Fraker DL, Karakousis GC (2018) Relationship between age and likelihood of lymph node metastases in patients with intermediate thickness melanoma (1.01–4.00 mm): a National Cancer Database study. J Am Acad Dermatol. https://doi.org/10.1016/j.jaad.2018.08.022
Leiter U, Stadler R, Mauch C, Hohenberger W, Brockmeyer N, Berking C, Sunderkotter C, Kaatz M, Schulte KW, Lehmann P, Vogt T, Ulrich J, Herbst R, Gehring W, Simon JC, Keim U, Martus P, Garbe C (2016) Complete lymph node dissection versus no dissection in patients with sentinel lymph node biopsy positive melanoma (DeCOG-SLT): a multicentre, randomised, phase 3 trial. Lancet Oncol 17:757–767. https://doi.org/10.1016/s1470-2045(16)00141-8
Moody JA, Ali RF, Carbone AC, Singh S, Hardwicke JT (2017) Complications of sentinel lymph node biopsy for melanoma—a systematic review of the literature. Eur J Surg Oncol 43:270–277
Sinnamon AJ, Sharon CE, Song Y, Neuwirth MG, Elder DE, Xu X, Chu EY, Ming ME, Fraker DL, Gimotty PA, Karakousis GC (2018) The prognostic significance of tumor-infiltrating lymphocytes for primary melanoma varies by sex. J Am Acad Dermatol 79:245–251. https://doi.org/10.1016/j.jaad.2018.02.066
Solari N, Bertoglio SAO, Boscaneanu A, Minuto M, Reina S, Palombo D, Bruzzi P, Cafiero F (2019) Sentinel lymph node biopsy in patients with malignant melanoma: analysis of post-operative complications. ANZ J Surg 89:1041–1044
Taylor RC, Patel A, Panageas KS, Busam KJ, Brady MS (2007) Tumor-infiltrating lymphocytes predict sentinel lymph node positivity in patients with cutaneous melanoma. J Clin Oncol 25:869–875. https://doi.org/10.1200/jco.2006.08.9755
Testori AAE, Blankenstein SA, van Akkooi ACJ (2019) Surgery for metastatic melanoma: an evolving concept. Curr Oncol Rep 21:98
Wong SL, Faries MB, Kennedy EB, Agarwala SS, Akhurst TJ, Ariyan C, Balch CM, Berman BS, Cochran A, Delman KA, Gorman M, Kirkwood JM, Moncrieff MD, Zager JS, Lyman GH (2018) Sentinel lymph node biopsy and management of regional lymph nodes in melanoma: American Society of Clinical Oncology and Society of Surgical Oncology Clinical Practice Guideline Update. J Clin Oncol 36:399–413. https://doi.org/10.1200/jco.2017.75.7724
Funding
This work was supported by the project of Epidemiology of melanoma (Ricerca Corrente 4.1; Italian Ministry of Health and by the Department of Epidemiology of the regional Health Service, Rome, Italy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fortes, C., Mastroeni, S., Caggiati, A. et al. High level of TILs is an independent predictor of negative sentinel lymph node in women but not in men. Arch Dermatol Res 313, 57–61 (2021). https://doi.org/10.1007/s00403-020-02067-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-020-02067-0