Abstract
Purpose
A well-balanced joint gap is necessary in Oxford unicompartmental knee arthroplasty (OUKA) to prevent mobile-bearing dislocation. While the gaps between 20° (extension) and 100° (flexion) are precisely adjusted using the incremental mill system, there has been insufficient evaluation of gaps in other angles. We hypothesized that the gap is not always the same in other angles. This retrospective study aimed to evaluate the gap in full-extension (0°), mid-flexion (60°) and deep flexion (130°) for comparison with those in extension and flexion gaps.
Methods
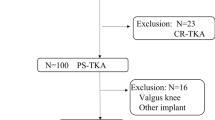
We evaluated 119 knees in 83 patients (51 females, 31 males, aged 71.9 years). The full-extension and mid-flexion gaps were compared with the extension gap, and the deep flexion gap was contrasted with the flexion gap. Each gap was classified into isometric, tight or loose, for evaluation of contributing factors.
Results
Although the full-extension gap tended to be isometric (45%), the mid-flexion tended to be tight (48%), whereas the deep-flexion was loose in most knees (84%) (P = 0.002). The tight mid-flexion and loose deep flexion gap pattern accounted for 44% of the total knees, especially so with smaller femoral components (P = 0.004).
Conclusion
Our results highlight the propensity of tight mid-flexion and loose flexion gap despite the adjustment of extension and flexion gaps in OUKA. Although the effect of such a minor gap imbalance is still unknown, the pattern was more prevalent in patients with smaller-sized femoral components. Use of a larger femoral component may equalize the gap throughout the motion arc.




Similar content being viewed by others
References
Ahn JH, Kang DM, Choi KJ (2017) Bilateral simultaneous unicompartmental knee arthroplasty versus unilateral total knee arthroplasty: a comparison of the amount of blood loss and transfusion, perioperative complications, hospital stay, and functional recovery. Orthop Traumatol Surg Res 103:1041–1045
Price AJ, Webb J, Topf H et al (2001) Rapid recovery after Oxford unicompartmental arthroplasty through a short incision. J Arthroplasty 16:970–976
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384:1437–1445
Goodfellow J, O’Connor J (1978) The mechanics of the knee and prosthesis design. J Bone Joint Surg Br 60–B:358–369
Price AJ, Short A, Kellett C et al (2005) Ten-year in vivo wear measurement of a fully congruent mobile bearing unicompartmental knee arthroplasty. J Bone Joint Surg Br 87:1493–1497
Kendrick BJL, Longino D, Pandit H et al (2010) Polyethylene wear in Oxford unicompartmental knee replacement a RETRIEVAL STUDY OF 47 BEARINGS. J Bone Joint Surg Br 92:367–373
Pandit H, Hamilton TW, Jenkins C et al (2015) The clinical outcome of minimally invasive phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. Bone Joint J 97–B:1493–1500
Choy WS, Kim KJ, Lee SK et al (2011) Mid-term results of oxford medial unicompartmental knee arthroplasty. Clin Orthop Surg 3:178–183
Kim KT, Lee S, Lee JI et al (2016) Analysis and treatment of complications after Unicompartmental Knee Arthroplasty. Knee Surg Relat Res 28:46–54
Ro K-H, Heo J-W, Lee D-H (2018) Bearing dislocation and progression of Osteoarthritis after Mobile-bearing Unicompartmental knee Arthroplasty Vary between Asian and Western patients: a Meta-analysis. Clin Orthop Relat Res 476:946–960
Sun X, Liu P, Lu F et al (2021) Bearing dislocation of mobile bearing unicompartmental knee arthroplasty in east Asian countries: a systematic review with meta-analysis. J Orthop Surg Res 16:28
Bae J-H, Kim JG, Lee S-Y et al (2020) Epidemiology of bearing dislocations after Mobile-Bearing Unicompartmental knee arthroplasty: Multicenter Analysis of 67 bearing dislocations. J Arthroplasty 35:265–271
ZimmerBiomet Oxford Partial Knee Microplasty Instrumentation Surgical Technique https://www.zimmerbiomet.com/content/dam/zimmer-biomet/medical-professionals/000-surgical-techniques/knee/oxford-partial-knee-microplasty-instrumentation-surgical-technique.pdf. Accessed 15 May 2022
Araki S, Hiranaka T, Okimura K et al (2022) Approximately 41% of knees have a looser gap in full extension than in 20° flexion after Oxford unicompartmental arthroplasty. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04350-3
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl 48:452–458
Takayama K, Matsumoto T, Muratsu H et al (2015) The tibia first technique with tensor measurement is useful to predict the soft tissue tension after implantation in unicompartmental knee arthroplasty. Int Orthop 39:667–671
Matsuzaki T, Matsumoto T, Muratsu H et al (2017) The contribution of intraoperative medial compartment stability to post-operative knee flexion angle in unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:272–276
Suzuki T, Ryu K, Kojima K et al (2019) The effect of posterior tibial slope on joint gap and range of knee motion in Mobile-Bearing Unicompartmental knee arthroplasty. J Arthroplasty 34:2909–2913
Price AJ, Svard U (2011) A second decade lifetable survival analysis of the oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res 469:174–179
Jamshed S, Shah R, Arooj A et al (2020) A novel radiographic technique to assess 180° rotational spin of the Oxford unicompartmental knee mobile bearing. J Orthop 21:438–443
Lisowski LA, Meijer LI, Van Den Bekerom MPJ et al (2016) Ten- to 15-year results of the Oxford Phase III mobile unicompartmental knee arthroplasty: a prospective study from a non-designer group. Bone Joint J. https://doi.org/10.1302/0301-620X.98B10.BJJ-2016-0474.R1. 98-B
Bitsch RG, von Keudell A, Losina E, Fitz W (2013) Good accuracy of the Phase III Oxford Mobile Bearing Unicompartmental Knee Instrumentation. Acta Orthop 84:406–409
Kang S-W, Kim K-T, Hwang Y-S et al (2020) Is Mobile-Bearing Medial Unicompartmental knee arthroplasty appropriate for Asian patients with the risk of Bearing. Dislocation? J Arthroplasty 35:1222–1227
Hiranaka T, Tanaka T, Fujishiro T et al (2020) A novel technique for Varus Tibial cutting for Oxford Unicompartmental Knee Arthroplasty. Clin Orthop Surg 12:554–557
Suda Y, Hiranaka T, Kamenaga T et al (2022) Varus placement of the tibial component of Oxford unicompartmental knee arthroplasty decreases the risk of postoperative tibial fracture. Bone Joint J 104–B:1118–1125
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This retrospective study was performed according to the Declaration of Helsinki and approved by the Ethics Committee of Takatsuki General Hospital.
Conflict of interest
The corresponding author is a paid presentor of Zimmer Biomet.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hiranaka, T., Kamachi, M., Hayashi, T. et al. Propensity of the tight mid-flexion and loose flexion gap despite the adjustment of extension and flexion gaps in Oxford unicompartmental knee arthroplasty: retrospective study. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-024-05377-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00402-024-05377-4