Abstract
Introduction
To understand the incidence of postoperative constipation and the risk factors of constipation in patients with lumbar interbody fusion, we constructed and verified the constipation risk prediction model, so as to provide reference for the prevention and treatment of postoperative constipation.
Methods
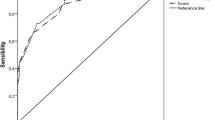
The data of patients undergoing lumbar interbody fusion in our hospital were retrospectively analyzed from December 2021 to December 2022. According to postoperative constipation, the patients were divided into constipation group and non-constipation group. Univariate logistic regression analysis and multivariate logistic regression analysis were used to determine independent risk factors for postoperative constipation. Based on independent risk factors, a nomogram was developed to predict the risk of constipation after lumbar interbody fusion. The prediction performance was assessed using receiver operating characteristic curve (ROC), calibration curve and decision curve analysis (DCA). Finally, bootstrapping method for internal validation was further evaluated the nomogram.
Results
A total of 282 patients participated in the study. 176 patients (62.41%) after lumbar interbody occurred constipation, and 106 patients were asymptomatic. Multivariate regression analysis showed independent risk factors, including the use of calcium channel blockers, polypharmacy, postoperative bed time, and constipation history. Multivariate regression analysis was used to establish the model. The C-index of the nomogram was 0.827 (95% CI 0.779–0.875), and the C-index of interval bootstrapping validation was 0.813 (95% CI 0.765–0.861), and the area under the AUC was 0.800. The nomogram showed good discrimination ability.
Conclusions
The use of calcium channel blockers, polypharmacy, postoperative bed time, and history of constipation are independent risk factors for postoperative constipation in patients undergoing lumbar interbody fusion. The constructed risk prediction model has good discriminative ability.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Reisener MJ, Pumberger M, Shue J, Girardi FP, Hughes AP (2020) Trends in lumbar spinal fusion-a literature review. J Spine Surg 6(4):752–761
Smith JT, Smith MS (2013) Does a preoperative bowel preparation reduce bowel morbidity and length of stay after scoliosis surgery? A randomized prospective study. J Pediatr Orthop 33(8):e69–e71
Crawford HA, Pillai AK, Upadhyay V (2005) Gastrointestinal morbidity following spinal surgery in children. J. Bone and Joint Surg. 87.
Prichard DO, Bharucha AE (2018) Recent advances in understanding and managing chronic constipation. F1000Res. 7:F1000 Faculty Rev-1640. Published 2018 Oct 15.
Berger V, Durand L, Grocq M (2010) Elimination intestinale à l’hôpital. Réflexion éthique sur sa prise en charge par les soignants [Constipation in the hospital. Ethical reflection on its care by the nursing staff]. Rech Soins Infirm 103:67–77
Jing D, Jia L (2019) Assessment of patients’ psychological state and self-efficacy associated with postoperative constipation after thoracolumbar fracture surgery. J Int Med Res 47(9):4215–4224
Yin H, Wang G, Wang J, Ma Y, Wu M, Qiu S, Su Q (2021) Prevalence and risk factor analysis of constipation after thoracolumbar vertebral compression fractures. Int J Gen Med 14:4117–4123
Stienen MN, Smoll NR, Hildebrandt G, Schaller K, Tessitore E, Gautschi OP (2014) Constipation after thoraco-lumbar fusion surgery. Clin Neurol Neurosurg 126:137–142
Komiya H, Umegaki H, Asai A, Kanda S, Maeda K, Nomura H, Kuzuya M (2019) Prevalence and risk factors of constipation and pollakisuria among older home-care patients. Geriatr Gerontol Int 19(4):277–281
Chapman S, Hungerford C (2015) Risk factors for and assessment of constipation. Nurs Older People 27(3):16–24
Mari A, Mahamid M, Amara H, Baker FA, Yaccob A (2020) Chronic constipation in the elderly patient: updates in evaluation and management. Korean J Fam Med 41(3):139–145
Yurtdaş G, Acar-Tek N, Akbulut G, Cemali Ö, Arslan N, Beyaz Coşkun A, Zengin FH (2020) Risk factors for constipation in adults: a cross-sectional study. J Am Coll Nutr 39(8):713–719
Ma X, Lu Q, Lu Y, Li X (2022) Risk and main contributing factors for constipation in patients with gastrointestinal cancer: a multicenter cross-sectional study in China. Support Care Cancer 30(10):8119–8127
Fosnes GS, Lydersen S, Farup PG (2012) Drugs and constipation in elderly in nursing homes: What is the relation? Gastroenterol Res Pract 2012:290231
Sobrado CW, Neto IJFC, Pinto RA, Sobrado LF, Nahas SC, Cecconello I (2021) Diagnosis and treatment of constipation: a clinical update based on the Rome IV criteria. J Coloproctol 38(02):137–144
Mason D, Tobias N, Lutkenhoff M, Stoops M, Ferguson D (2004) The APN’s guide to pediatric constipation management. Nurse Pract 29(7):13–23
Costilla VC, Foxx-Orenstein AE (2014) Constipation: understanding mechanisms and management. Clin Geriatr Med 30(1):107–115
Rao SS, Go JT (2010) Update on the management of constipation in the elderly: new treatment options. Clin Interv Aging 5:163–171
Gallagher P, O'Mahony D (2009) Constipation in old age.Best practice & research. Clinical gastroenterology 23(6): 875–879.
Holman C, Roberts S, Nicol M (2008) Preventing and treating constipation in later life. Nurs Older People 20(5):22–24
Toner F, Claros E (2012) Preventing, assessing, and managing constipation in older adults. Nursing 42(12):32–40
Rasmussen LS, Pedersen PU (2010) Constipation and defecation pattern the first 30 days after thoracic surgery. Scand J Caring Sci 24(2):244–250
Desouza MS (2002) Effectiveness of nursing interventions in alleviating perceived problems among orthopaedic patients. J Orthopaedic Nursing 6(4):211–219
Gallegos-Orozco JF, Foxx-Orenstein AE, Sterler SM, Stoa JM (2012) Chronic constipation in the elderly. Am J Gastroenterol 107(1):18–26
Al Nou'mani J, Al Alawi AM, Al-Maqbali JS, Al Abri N, Al Sabbri M (2023) Prevalence, Recognition, and Risk Factors of Constipation among Medically Hospitalized Patients: A Cohort Prospective Study. Medicina (Kaunas) 59(7):1347. Published 2023 Jul 23.
Elliott WJ, Ram CV (2011) Calcium channel blockers. J Clin Hypertens (Greenwich) 13(9):687–689
Traube M, McCallum RW (1984) Calcium-channel blockers and the gastrointestinal tract. American College of Gastroenterology's Committee on FDA related matters. Am J Gastroenterol 79(11):892–896.
Inman BL, Long B (2023) Thyrotoxicosis. Emerg Med Clin North Am 41(4):759–774
Sayuk GS, Yu QT, Shy C (2023) Management of Constipation in Hospitalized Patients. J Clin Med 12(19):6148. Published 2023 Sep 23.
Funding
Supported by the Chongqing Medical Scientific Research Project (Grant No. 2024WSJK057).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki and the study was approved by the Medical Ethics Committee of the Second affiliated hospital of Chongqing Medical University.
Informed consent
Written informed consent was obtained from the parents.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, M., Cheng, S., Zhong, D. et al. Development and validation of a nomogram to predict the risk of constipation after lumbar interbody fusion surgery. Arch Orthop Trauma Surg 144, 1907–1916 (2024). https://doi.org/10.1007/s00402-024-05256-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-024-05256-y