Abstract
Introduction
The role of different femoral head materials for total hip arthroplasty (THA) has been widely studied in the context of wear properties and corrosion. Cobalt chrome (CoCr) femoral heads are commonly used as a standard of comparison to other materials such as ceramic and oxidized zirconium (OxZi). This study aims to evaluate the impact of femoral head material on clinical outcomes in elective primary THA patients.
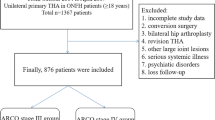
Methods
Retrospective analysis of THA patients within the Medicare claims database between October 2017 and September 2020 using diagnosis-related group codes was conducted. Information collected included sex, age, Charlson Comorbidity Index, and femoral head type. Patients with CoCr femoral heads were compared against patients with either OxZi or ceramic femoral heads using 1:1 propensity score matching. Z-testing and Chi-square analysis were used to determine between-group significance.
Results
In total, 112,960 elective THA patients were included, with 56,480 in OxZi or ceramic and 56,480 in CoCr. Readmission rates were lower in patients that received OxZi or ceramic femoral heads at 30-day (p < 0.0001), 60-day (p < 0.0001), and 90-day postoperatively (p < 0.0001) compared to CoCr. Mortality rates were also lower in patients that received OxZi or ceramic femoral heads at 30-day (p = 0.004), 60-day (p = 0.018), and 90-day postoperatively (p = 0.009) compared to CoCr.
Conclusion
CoCr femoral heads had higher rates of readmissions and mortality compared to OxZi or ceramic. Further analysis of bearing surface combinations and sub-group analyses to determine significance between-group differences is needed.
Level III evidence
Retrospective analysis.

Similar content being viewed by others
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Malahias M-A, Atrey A, Gu A, Chytas D, Nikolaou VS, Waddell JP (2019) Is oxidized zirconium femoral head superior to other bearing types in total hip arthroplasty? A systematic review and meta-analysis. J Arthroplasty 34(8):1844–1852. https://doi.org/10.1016/j.arth.2019.03.072
Bourne RB, Barrack R, Rorabeck CH, Salehi A, Good V (2005) Arthroplasty options for the young patient: oxinium on cross-linked polyethylene. Clin Orthop 441(NA):159–167. https://doi.org/10.1097/01.blo.0000193813.08458.e2
Good V, Ries M, Barrack R, Widding K, Hunter G, Heuer D (2003) Reduced wear with oxidized zirconium femoral heads. J Bone Jt Surg. 85(suppl_4):105–110
Ries M, Salehi A, Widding K, Hunter G (2002) Polyethylene wear performance of oxidized zirconium and cobalt-chromium knee components under abrasive conditions. J Bone Jt Surg. 84(suppl_2):S129–S135
Cartner J, Aldinger P, Li C, Collins D (2017) Characterization of femoral head taper corrosion features using a 22-year retrieval database. HSS J ® 13(1):35–41. https://doi.org/10.1007/s11420-016-9517-5
Garvin KL, Hartman CW, Mangla J, Murdoch N, Martell JM (2009) Wear analysis in THA utilizing oxidized zirconium and crosslinked polyethylene. Clin Orthop 467(1):141–145. https://doi.org/10.1007/s11999-008-0544-5
Nam D, Keeney JA, Nunley RM, Johnson SR, Clohisy JC, Barrack RL (2015) Metal ion concentrations in young, active patients following total hip arthroplasty with the use of modern bearing couples. J Arthroplasty 30(12):2227–2232. https://doi.org/10.1016/j.arth.2015.06.025
Jassim SS, Patel S, Wardle N et al (2015) Five-year comparison of wear using oxidised zirconium and cobalt–chrome femoral heads in total hip arthroplasty: a multicentre randomised controlled trial. Bone Jt J 97-B(7):883–889. https://doi.org/10.1302/0301-620X.97B7.35285
Bozic KJ, Ong K, Kurtz S et al (2016) Short-term risk of revision THA in the medicare population has not improved with time. Clin Orthop Relat Res 474(1):156–163. https://doi.org/10.1007/s11999-015-4520-6
Centers for Medicare and Medicaid Service. Standard Analytical Files—LDS. https://www.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/LimitedDataSets/StandardAnalyticalFiles.html. Accessed 22 June 2022
Nandi S, Austin MS (2017) Choosing a femoral head: a survey study of academic adult reconstructive surgeons. J Arthroplasty 32(5):1530–1534. https://doi.org/10.1016/j.arth.2016.12.009
Wyles CC, Jimenez-Almonte JH, Murad MH et al (2015) There are no differences in short- to mid-term survivorship among total hip-bearing surface options: a network meta-analysis. Clin Orthop Relat Res 473(6):2031–2041. https://doi.org/10.1007/s11999-014-4065-0
Cafri G, Paxton EW, Love R, Bini SA, Kurtz SM (2017) Is there a difference in revision risk between metal and ceramic heads on highly crosslinked polyethylene liners? Clin Orthop Relat Res 475(5):1349–1355. https://doi.org/10.1007/s11999-016-4966-1
Schwarzkopf R, Behery OA, Yu H, Suter LG, Li L, Horwitz LI (2019) Patterns and costs of 90-day readmission for surgical and medical complications following total hip and knee arthroplasty. J Arthroplasty 34(10):2304–2307. https://doi.org/10.1016/j.arth.2019.05.046
Singh JA, Cleveland JD (2018) Medicaid or Medicare insurance payer status and household income are associated with outcomes after primary total hip arthroplasty. Clin Rheumatol 37(9):2489–2496. https://doi.org/10.1007/s10067-018-4126-y
Harris IA, Hatton A, Steiger R, Lewis P, Graves S (2020) Declining early mortality after hip and knee arthroplasty. ANZ J Surg 90(1–2):119–122. https://doi.org/10.1111/ans.15529
Parvizi J, Johnson BG, Rowland C, Ereth MH, Lewallen DG (2001) Thirty-day mortality after elective total hip arthroplasty. J Bone Jt Surg-Am 83(10):1524–1528. https://doi.org/10.2106/00004623-200110000-00010
Tarity TD, Herz AL, Parvizi J, Rothman RH (2006) Ninety-day mortality after hip arthroplasty. J Arthroplasty 21(6):60–64. https://doi.org/10.1016/j.arth.2006.05.016
Jameson SS, Baker PN, Mason J et al (2013) Independent predictors of failure up to 7.5 years after 35 386 single-brand cementless total hip replacements: a retrospective cohort study using National Joint Registry data. Bone Jt J. 95-B(6):747–757. https://doi.org/10.1302/0301-620X.95B6.31378
Jameson SS, Baker PN, Mason J et al (2012) The design of the acetabular component and size of the femoral head influence the risk of revision following 34 721 single-brand cemented hip replacements: a retrospective cohort study of medium-term data from a National Joint Registry. J Bone Joint Surg Br 94-B(12):1611–1617. https://doi.org/10.1302/0301-620X.94B12.30040
Jameson SS, Mason J, Baker P et al (2014) A Comparison of surgical approaches for primary hip arthroplasty: a cohort study of patient reported outcome measures (PROMs) and early revision using linked national databases. J Arthroplasty 29(6):1248-1255.e1. https://doi.org/10.1016/j.arth.2013.11.027
Lindgren JV, Wretenberg P, Kärrholm J, Garellick G, Rolfson O (2014) Patient-reported outcome is influenced by surgical approach in total hip replacement: a study of the Swedish Hip Arthroplasty Register including 42 233 patients. Bone Jt J 96-B(5):590–596. https://doi.org/10.1302/0301-620X.96B5.32341
Kostensalo I, Junnila M, Virolainen P et al (2013) Effect of femoral head size on risk of revision for dislocation after total hip arthroplasty: a population-based analysis of 42,379 primary procedures from the Finnish Arthroplasty Register. Acta Orthop 84(4):342–347. https://doi.org/10.3109/17453674.2013.810518
Furnes O, Paxton E, Cafri G et al (2014) Distributed analysis of hip implants using six national and regional registries: comparing metal-on-metal with metal-on-highly cross-linked polyethylene bearings in cementless total hip arthroplasty in young patients. J Bone Jt Surg 96(suppl 1):25–33. https://doi.org/10.2106/JBJS.N.00459
Thien TM, Chatziagorou G, Garellick G et al (2014) Periprosthetic femoral fracture within two years after total hip replacement: analysis of 437,629 operations in the Nordic Arthroplasty Register Association Database. J Bone Jt Surg. 96(19):e167. https://doi.org/10.2106/JBJS.M.00643
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
CS, NM, VS, PS, TN, and KH have nothing to disclose. RS reports being a paid consultant for Smith & Nephew, Intellijoint, and Zimmer; has stock options in Gauss Surgical and PSI, and receives IP royalties from Smith & Nephew, outside the submitted work.
Ethical approval
The present study was approved from human subjects review by our institutional review board (IRB).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sicat, C.S., Singh, V., Muthusamy, N. et al. Role of femoral head material on readmission and mortality rates following elective primary total hip arthroplasty in Medicare patients. Arch Orthop Trauma Surg 144, 459–464 (2024). https://doi.org/10.1007/s00402-023-05027-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05027-1