Abstract
Introduction
It is preferable to reduce postoperative excessive rotational mismatch between the femur and tibia that causes poor clinical results following total knee arthroplasty (TKA). The aim of this study is to compare postoperative rotational mismatches and clinical outcomes with mobile- and fixed-bearing prostheses.
Materials and methods
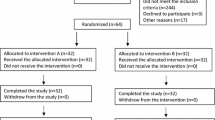
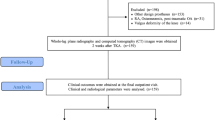
This study classified 190 TKAs into two groups equally by propensity score matching: mobile-bearing group (n = 95) and fixed-bearing group (n = 95). Computed tomography images of the whole leg were taken at 2 weeks postoperatively. The component alignments, rotational mismatches between the femur and tibia, and rotations among components were measured three-dimensionally. The knee range of motion, New Knee Society Score (KSS) subjective sores, and Forgotten Joint Score (FJS-12) were assessed at the final follow-up.
Results
Rotational mismatch between the femur and tibia was significantly less in the mobile- (− 0.8° ± 7.3°) than in the fixed-bearing (3.3° ± 8.5°, p < 0.001) group. New KSS functional activity score was significantly poorer in patients with excessive rotational mismatch (61.3 ± 21.4) than in those without it (49.5 ± 20.6, p = 0.02). Comparing mobile-bearing prosthesis, the use of fixed-bearing prosthesis was a risk factor for postoperative excessive rotational mismatch (odds ratio: 2.32, p = 0.03).
Conclusion
When compared to a fixed-bearing prosthesis, TKA using a mobile-bearing prosthesis could suppress the postoperative rotational mismatch between the femur and tibia that causes poor subjective functional activity score. However, since this study was conducted for PS-TKA, the results might not be applicable to other models.





Similar content being viewed by others
Data availability
The data is stored in a data repository.
References
Ritter MA, Davis KE, Davis P et al (2013) Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Joint Surg Am 95:126–131. https://doi.org/10.2106/JBJS.K.00607
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br 92:1238–1244. https://doi.org/10.1302/0301-620X.92B9.23516
Verlinden C, Uvin P, Labey L et al (2010) The influence of malrotation of the femoral component in total knee replacement on the mechanics of patellofemoral contact during gait. J Bone Joint Surg Br 92:737–742. https://doi.org/10.1302/0301-620X.92B5.22603
Panni AS, Ascione F, Rossini M et al (2018) Tibial internal rotation negatively affects clinical outcomes in total knee arthroplasty: a systematic review. Knee Surg Sport Traumatol Arthrosc 26:1636–1644. https://doi.org/10.1007/s00167-017-4823-0
Ueyama H, Minoda Y, Sugama R et al (2020) Malrotation of the fixed-bearing posterior stabilized total knee prosthesis causes a postoperative rotational mismatch between the femur and tibia. Knee Surg Sport Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-05864-2
Tjørnild M, Søballe K, Hansen PM et al (2015) Mobile- vs. fixed-bearing total knee replacement. Acta Orthop 86:208–214. https://doi.org/10.3109/17453674.2014.968476
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 46:399–424. https://doi.org/10.1080/00273171.2011.568786
Ueyama H, Minoda Y, Sugama R et al (2019) Two-dimensional measurement misidentifies alignment outliers in total knee arthroplasty: a comparison of two- and three-dimensional measurements. Knee Surg Sport Traumatol Arthrosc 27:1497–1503. https://doi.org/10.1007/s00167-018-5175-0
Berger RA, Rubash HE, Seel MJ et al (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199301000-00008
Akagi M, Oh M, Nonaka T et al (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-200403000-00030
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-198911000-00004
Scuderi GR, Bourne RB, Noble PC et al (2012) The new knee society knee scoring system. Clin Orthop Relat Res 470:3–19. https://doi.org/10.1007/s11999-011-2135-0
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “forgotten joint” as the ultimate goal in joint arthroplasty. J Arthroplasty 27:430–436. https://doi.org/10.1016/j.arth.2011.06.035
Minoda Y, Iwaki H, Ikebuchi M et al (2012) The flexion gap preparation does not disturb the modified gap technique in posterior stabilized total knee arthroplasty. Knee 19:832–835. https://doi.org/10.1016/j.knee.2012.03.007
Ueyama H, Minoda Y, Sugama R et al (2019) An accelerometer-based portable navigation system improved prosthetic alignment after total knee arthroplasty in 3D measurements. Knee Surg Sport Traumatol Arthrosc 27:1580–1586. https://doi.org/10.1007/s00167-018-5082-4
Gøttsche D, Gromov K, Viborg PH et al (2019) Weight affects survival of primary total knee arthroplasty: study based on the Danish Knee Arthroplasty Register with 67,810 patients and a median follow-up time of 5 years. Acta Orthop 90:60–66. https://doi.org/10.1080/17453674.2018.1540091
Okamoto N, Nakamura E, Nishioka H et al (2014) In vivo kinematic comparison between mobile-bearing and fixed-bearing total knee arthroplasty during step-up activity. J Arthroplasty 29:2393–2396. https://doi.org/10.1016/j.arth.2014.02.022
Angibaud LD, Dai Y, Liebelt RA et al (2015) Evaluation of the accuracy and precision of a next generation computer-assisted surgical system. Clin Orthop Surg 7:225–233. https://doi.org/10.4055/cios.2015.7.2.225
Kuriyama S, Hyakuna K, Inoue S et al (2014) Tibial rotational alignment was significantly improved by use of a CT-navigated control device in total knee arthroplasty. J Arthroplasty 29:2352–2356. https://doi.org/10.1016/j.arth.2014.06.016
Kawahara S, Okazaki K, Matsuda S et al (2014) Internal rotation of femoral component affects functional activities after TKA–survey with the 2011 Knee Society Score. J Arthroplasty 29:2319–2323. https://doi.org/10.1016/j.arth.2013.11.017
Jónasson G, Helgason A, Ingvarsson Þ et al (2016) The effect of tibial rotation on the contribution of medial and lateral hamstrings during isometric knee flexion. Sports Health 8:161–166. https://doi.org/10.1177/1941738115625039
Saç A, Taşmektepligil MY (2018) Correlation between the Q angle and the isokinetic knee strength and muscle activity. Turkish J Phys Med Rehabil 64:308–313. https://doi.org/10.5606/tftrd.2018.2366
Giesinger K, Hamilton DF, Jost B et al (2014) Comparative responsiveness of outcome measures for total knee arthroplasty. Osteoarthr Cartil 22:184–189. https://doi.org/10.1016/j.joca.2013.11.001
Joice MG, Bhowmick S, Amanatullah DF (2017) Perioperative physiotherapy in total knee arthroplasty. Orthopedics 40:e765–e773. https://doi.org/10.3928/01477447-20170518-03
Zeni JA, Snyder-Mackler L (2010) Early postoperative measures predict 1- and 2-year outcomes after unilateral total knee arthroplasty: importance of contralateral limb strength. Phys Ther 90:43–54. https://doi.org/10.2522/ptj.20090089
Acknowledgements
We appreciate the contributions from all group members in the medical stuff at each institution.
Funding
This study was not supported by any funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ueyama, H., Minoda, Y., Sugama, R. et al. Mobile-bearing prosthesis suppresses the postoperative rotational mismatch and improves patient-reported outcome measurements better than fixed-bearing prosthesis: rotational analysis by 3D measurement in total knee arthroplasty. Arch Orthop Trauma Surg 143, 6781–6790 (2023). https://doi.org/10.1007/s00402-023-04971-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04971-2