Abstract
Introduction
Surgical smoke generated through the use of electrical surgical devices poses a risk to the surgeon, medical personnel in the operating room, and the patient by exposing them to environmentally hazardous particulate matter. Previous investigation has shown that surgical smoke leads to an increased risk of pulmonary conditions, circulatory disorders, and irritation of the eyes, nose, and throat. Transmission of infectious disease can occur through inhalation of viral particles, and the presence of carcinogens are also of major concern. The deleterious effects of surgical smoke are well documented in several subspecialties, namely dermatology and general surgery, but there has been little discussion on the topic amongst orthopedic surgeons.
Methods
A non-systematic review of the literature was completed with the aim of identifying the major categories of adverse health effects associated with surgical smoke inhalation and offering recommendations to reduce these hazards in the orthopedic surgical community.
Results
Three primary categories of risk associated with surgical smoke inhalation were identified: inflammation, viral/bacterial transmission, and carcinogenicity. In addition, strategies for mitigating risk and best practice recommendations were explored.
Conclusion
Surgical smoke is an under-recognized occupational hazard within the orthopedic surgery literature. There are several strategies which can be employed to reduce risk. Further investigation is needed to understand the long-term impact of these risks, as well as what can be done to improve the practicality and compliance with protective measures.
Similar content being viewed by others
Data availability
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
References
Ryu RC, Behrens PH, Malik AT, Lester JD, Ahmad CS. Are we putting ourselves in danger? Occupational hazards and job safety for orthopaedic surgeons. J Orthop. 2021;24:96–101. Published 2021 Feb 20. https://doi.org/10.1016/j.jor.2021.02.023
Kugelman D, Weppler CG, Warren CF, Lajam CM (2022) Occupational hazards of orthopedic surgery exposures: infection, smoke, and noise. J Arthroplasty 37(8):1470–1473. https://doi.org/10.1016/j.arth.2022.03.034
Patel K, Judd H, Harm RG, Spanyer J (2022) Occupational hazards for the practicing orthopaedic surgeon: a standard review. J Am Acad Orthop Surg 30(7):e607–e616. https://doi.org/10.5435/JAAOS-D-21-00612
Vajapey SP, Li M, Glassman AH. Occupational hazards of orthopaedic surgery and adult reconstruction: a cross-sectional study. J Orthop. 2021;25:23–30. Published 2021 Apr 2. doi:https://doi.org/10.1016/j.jor.2021.03.026
Liu Y, Song Y, Hu X et al (2019) Awareness of surgical smoke hazards and enhancement of surgical smoke prevention among the gynecologists. J Cancer 10(12):2788–2799
Limchantra IV, Fong Y, Melstrom KA (2019) Surgical smoke exposure in operating room personnel: a review. JAMA Surg 154(10):960–967
Choi SH, Kwon TG, Chung SK et al (2014) Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg Endosc 28(8):2374–2380
Li CI, Chou YH, Pai JY, Chen CH, Chiang MC. Investigating surgical smoke in otolaryngology operating rooms. Sci Rep. 2022;12(1):1719. Published 2022 Feb 2. https://doi.org/10.1038/s41598-022-05701-1
Swerdlow BN (2020) Surgical smoke and the anesthesia provider. J Anesth 34(4):575–584. https://doi.org/10.1007/s00540-020-02775-x
Kokosa JM, Eugene J (1989) Chemical composition of laser-tissue interaction smoke plume. J Laser Appl 1(3):59–63
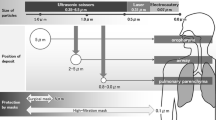
Oberdöster G, Oberdöster E, Oberdöster J (2005) Nanotoxicology an emerging discipline evolving from studies of ultrafine particles. Environ Health Perspec 113(7):823–839
Bruske-Hohlfeld I, Preissler G, Jauch KW et al (2008) Surgical smoke and ultrafine particles. J Occup Med Toxicol 3:31
Kunachak S, Sobhon P (1998) The potential alveolar hazard of carbon dioxide laser-induced smoke. J Med Assoc Thai 81(4):278–282
Yeganeh A, Hajializade M, Sabagh AP, Athari B, Jamshidi M, Moghtadaei M. Analysis of electrocautery smoke released from the tissues frequently cut in orthopedic surgeries. World J Orthop. 2020;11(3):177–183. Published 2020 Mar 18. https://doi.org/10.5312/wjo.v11.i3.177
Ulmer BC (2008) The hazards of surgical smoke. AORN J 87(4):721–738
Barrett WL, Garber SM: Surgical smoke: a review of the literature. Is this just a lot of hot air? Surg Endosc 2003;17(6):979 –87.
Steege AL, Boiano JM, Sweeny MH (2016) Secondhand smoke in the operating room? Precautionary practices lacking for surgical smoke. Am J Ind Med 59(11):1020–1031
Canicoba ARB, Poveda VB (2022) Surgical smoke and biological symptoms in healthcare professionals and patients: a systematic review. J Perianesth Nurs 37(1):130–136. https://doi.org/10.1016/j.jopan.2021.06.106
Alp E, Bijl D, Bleichrodt RP, Hansson B et al (2006) Surgical smoke and infection control. J Hosp Infect 62(1):1–5
Ball K (2010) Compliance with surgical smoke evacuation guidelines: implications for practice. Aorn J 92(2):142–149
Bernstein JA, Alexis N, Bacchus H, Bernstein IL et al (2008) The health effects of nonindustrial indoor air pollution. J Allergy Clin Immunol 121(3):585–591
Okoshi K, Kobayashi K, Kinoshita K, Tomizawa Y et al (2015) Health risks associated with exposure to surgical smoke for surgeons and operating room personnel. Surg Today 45(8):957–965
Baggish MS, Baltoyannis P, Sze E (1988) Protection of the rat lung from the harmful effects of laser smoke. Lasers Surg Med 8(3):248–253
Baggish MS, Elbakry M (1987) The effects of laser smoke on the lungs of rats. Am J Obstet Gynecol 156(5):1260–1265
Capizzi PJ, Clay RP, Battey MJ (1998) Microbiologic activity in laser resurfacing plume and debris. Lasers Surg Med 23(3):172–174
Butler D: Health Risks of Indoor Exposure to Particulate Matter: Workshop Summary. Washington, DC: National Academies Press (US); 2016 Sept 26.
Hedley AK: Surgical Smoke Almost Killed Me. Outpatient Surgery Magazine. 2018;32–39.
Taravella MJ, Weinberg A, May M et al (1999) Live virus survives excimer laser ablation. Ophthalmology 106(8):1498–1499
K HD, Kim SH, Seo YS, et al: Detecting hepatitis B virus in surgical smoke emitted during laparoscopic surgery. Ocup Environ Med 2016;73(12):857–863.
Zhou Q, Hu X, Zhou J et al (2019) Human papillomavirus DNA in surgical smoke during cervical loop electrosurgical excision procedures and its impact on the surgeon. Cancer Manag Res 11:3643–3654
Garden GM, O’Banion K, Bakus AD et al (2002) Viral disease transmitted by laser-generated plume (aerosol). Arch Dermat 138(10):1303–1307
Tomita Y, Mihashi S, Nagata K et al (1981) Mutagenicity of smoke condensates induced by CO2-laser irradiation and electrocauterization. Mutat Res 89(2):145–149
Hill DS, O’Neill JK, Powell RJ, Oliver DW. Surgical smoke - a health hazard in the operating theatre: a study to quantify exposure and a survey of the use of smoke extractor systems in UK plastic surgery units. J Plast Reconstr Aesthet Surg. 2012;65(7):911–916.
Al Sahaf OS, Vega-Carrascal I, Cunningham FO et al (2007) Chemical composition of smoke produced by high-frequency electrosurgery. Ir J Med Sci 176(3):229–232
Hui Y, Yan J (2018) Effect of electrosurgery in the operating room on surgeons’ blood indices: a simulation model and experiment on rabbits. J Int Med Res 46(12):5245–5256
Douglas JDM, McLean N, Horsley C et al (2020) COVID-19: smoke testing of surgical mask and respirators. Occup Med 70(8):556–563
Zakka K, Erridge S, Chidambaram S et al (2020) Electrocautery, diathermy, and surgical energy devices: are surgical teams at risk during the COVID-19 pandemic? Ann Surg 272(3):e257–e262. https://doi.org/10.1097/SLA.0000000000004112
Matta I, Laganà AS, Ghabi E et al (2022) COVID-19 transmission in surgical smoke during laparoscopy and open surgery: a systematic review. Minim Invasive Ther Allied Technol 31(5):690–697. https://doi.org/10.1080/13645706.2021.1982728
Chapman LW, Korta DZ, Lee PK et al (2017) Awareness of surgical smoke risks and assessment of safety practices during electrosurgery among US dermatology residents. JAMA Dermatol 153(5):467–468
Edwards BE, Rieman RE (2012) Comparison of current and past surgical smoke control practices. AORN J 95(3):337–350
Oberg T, Brosseau LM (2008) Surgical mask filter and fit performance. Am J Infect Control 36(4):276–282
Makison Booth C, Clayton M, Crook B et al (2013) Effectiveness of surgical masks against influenza bioaerosols. J Hosp Infect 84(1):22–26
Benson SM, Novak DA, Ogg MJ (2013) Proper use of surgical n95 respirators and surgical masks in the OR. Aorn j 97(4):457–467
Doyle C: Surgical Smoke: A Potential Risk Too Real to Ignore Any Longer. General Surgery News. Sept 22, 2020
Funding
There were no sources of funding for the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Brown is a paid consultant for Depuy/Synthes and Corin USA and board or committee member of American Academy of Orthopaedic Surgeons. Dr. Schiff is a paid consultant for DJ Orthopaedics, Regeneration Technologies, Inc., Restor3D, and Stryker. All other authors have no competing interests to declare. There were no sources of funding for this review.
Ethical approval
This manuscript does not involve Protected Health Information (PHI); therefore, Institution Review Board (IRB) approval was not indicated.
Informed consent
This manuscript did not involve direct patient information or interaction; therefore, no informed consent was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
LeDuc, R., Eikani, C., Dickens, B. et al. Surgical smoke and the orthopedic surgeon: a non-systematic review of the hazards and strategies for mitigating risk. Arch Orthop Trauma Surg 143, 6975–6981 (2023). https://doi.org/10.1007/s00402-023-04967-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04967-y