Abstract
Introduction
To systematically review and analyze the safety and effectiveness of ERAS in older patients undergoing orthopedic surgeries.
Materials and methods
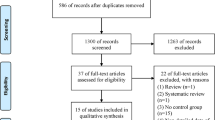
We searched PubMed, EMBASE, CINAHL, MEDLINE (Ovid), Web of Science, the Cochrane Library, and other databases to identify all randomized controlled studies and cohorts. We used the Cochrane Risk of Bias Assessment Tool and the Newcastle‒Ottawa Scale to assess the study quality. A meta-analysis was performed using the inverse variance weighting method.
Results
This study included 15 studies involving a total of 2591 older patients undergoing orthopedic surgeries with 1480 in the ERAS group. The ERAS group had a lower incidence of postoperative complications than the control group (RR 0.52; 95% CI 0.42–0.65). Length of stay was 3.37 days lower in the ERAS group than in the control group (P < 0.01). And the ERAS protocol reduced the patient’s postoperative VAS score (P < 0.01). Meanwhile, there was a lack of evidence of significant differences between the ERAS group and the control group in total bleeding and 30-day readmission rate.
Conclusions
The implementation of the ERAS program in older patients undergoing orthopedic surgeries is safe and effective. However, there is still a lack of standardization of protocols across institutions and centers for orthopedic surgery for older patients. Identifying ERAS components that are beneficial to older patients and developing ERAS protocols that are appropriate for older adults may further improve outcomes.



Similar content being viewed by others
Data availability
The authors declare that the data supporting the findings of this study are available within the article (and its supplementary information files).
References
Tao J, Yan Z, Bai G, Zhang H, Li J (2023) Enhanced recovery after surgery rehabilitation protocol in the perioperative period of orthopedics: a systematic review. J Pers Med 13(3):421. https://doi.org/10.3390/jpm13030421
Kowa CY, Jin Z, Gan TJ (2022) Framework, component, and implementation of enhanced recovery pathways. J Anesth 36(5):648–660. https://doi.org/10.1007/s00540-022-03088-x
Salamanna F, Contartese D, Brogini S, Visani A, Martikos K, Griffoni C et al (2022) Key components, current practice and clinical outcomes of ERAS programs in patients undergoing orthopedic surgery: a systematic review. J Clin Med 11(14):4222. https://doi.org/10.3390/jcm11144222
Martina K, Hunter DJ, Salmon LJ, Roe JP, Dowsey MM (2022) Surgery for osteoarthritis: total joint arthroplasty, realistic expectations of rehabilitation and surgical outcomes: a narrative review. Clin Geriatr Med 38(2):385–396. https://doi.org/10.1016/j.cger.2021.11.009
Wainwright TW, Gill M, McDonald DA, Middleton RG, Reed M, Sahota O et al (2020) Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop 91(1):3–19. https://doi.org/10.1080/17453674.2019.1683790
Debono B, Wainwright TW, Wang MY, Sigmundsson FG, Yang MMH, Smid-Nanninga H et al (2021) Consensus statement for perioperative care in lumbar spinal fusion: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Spine J 21(5):729–752. https://doi.org/10.1016/j.spinee.2021.01.001
Morrell AT, Layon DR, Scott MJ, Kates SL, Golladay GJ, Patel NK (2021) Enhanced recovery after primary total hip and knee arthroplasty: a systematic review. J Bone Joint Surg Am 103(20):1938–1947. https://doi.org/10.2106/jbjs.20.02169
Court-Brown CM, McQueen MM (2016) Global forum: fractures in the elderly. J Bone Joint Surg Am 98(9):e36. https://doi.org/10.2106/jbjs.15.00793
Fischer K (2019) Geriatric patients in orthopedics=Der geriatrische Patient in der Orthopädie. Orthopade 48(5):441–450. https://doi.org/10.1007/s00132-019-03723-8
Greenstein AS, Gorczyca JT (2019) Orthopedic surgery and the geriatric patient. Clin Geriatr Med 35(1):65–92. https://doi.org/10.1016/j.cger.2018.08.007
Song K, Zhu B, Yao Y, Jiang Q, Xiong J, Shi H (2022) Incidence and risk factors of preoperative deep vein thrombosis in patients with intertrochanteric fractures: a retrospective study. J Orthop Surg Res 17(1):375. https://doi.org/10.1186/s13018-022-03268-1
de Haan E, van Rijckevorsel V, Bod P, Roukema GR, de Jong L (2023) Delirium after surgery for proximal femoral fractures in the frail elderly patient: risk factors and clinical outcomes. Clin Interv Aging 18:193–203. https://doi.org/10.2147/cia.S390906
Gupta P, Quan T, Zimmer ZR (2022) Thirty-day morbidity and mortality following revision total shoulder arthroplasty in octogenarians. Should Elb 14(4):402–409. https://doi.org/10.1177/17585732211027334
Kehlet H (2020) Enhanced postoperative recovery: good from afar, but far from good? Anaesthesia 75(Suppl 1):e54–e61. https://doi.org/10.1111/anae.14860
Deytrikh A, Tou S, Bergamaschi R (2015) Tailor-made enhanced recovery programme for older patients. Tech Coloproctol 19(11):671–672. https://doi.org/10.1007/s10151-015-1376-4
Hu ZC, He LJ, Chen D, Li XB, Feng ZH, Fu CW et al (2019) An enhanced recovery after surgery program in orthopedic surgery: a systematic review and meta-analysis. J Orthop Surg Res 14(1):77. https://doi.org/10.1186/s13018-019-1116-y
Xiuhong BAO, Yanning HU, Suxian Z, Lianqi FU, Sisi YAN (2019) A meta-analysis of fast-track surgery in perioperative pain management of elderly patients with hip fracture. Nurs Integr Tradit Chin Western Med 5(6):28–32. https://doi.org/10.11997/nitcwm.201906008
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ et al (2022) Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane www.training.cochrane.org/handbook
Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M et al (2018) The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. The Ottawa Hospital http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Jiang H-H, Jian X-F, Shangguan Y-F, Qing J, Chen L-B (2019) Effects of enhanced recovery after surgery in total knee arthroplasty for patients older than 65 years. Orthop Surg 11(2):229–235. https://doi.org/10.1111/os.12441
Sura-amonrattana U, Tharmviboonsri T, Unnanuntana A, Tantigate D, Srinonprasert V (2021) Evaluation of the implementation of multidisciplinary fast-track program for acute geriatric hip fractures at a University Hospital in resource-limited settings. BMC Geriatr 21(1):1–11. https://doi.org/10.1186/s12877-021-02509-y
Li H, Liu Y, Li Q, Fan JL, Gan L, Wang YX (2020) Effects of a fast track surgery nursing program in perioperative care of older patients with a hip fracture. Eur Geriatr Med 11(4):519–525. https://doi.org/10.1007/s41999-020-00298-y
Peng N, Li J (2021) Application effect of case management mode combined with ERAS in elderly patients with hip fracture. Evid Based Complement Alternat Med (eCAM) 2021:1–7. https://doi.org/10.1155/2021/1175020
Ping H, Ling X, Xue YW, Dong FH (2021) Effect of ERAS combined with comfortable nursing on quality of life and complications in femoral neck fractures of the aged people. Evid Based Complement Altern Med. https://doi.org/10.1155/2021/8753076
Tian Z, Pang D, Liu H, Zhou L, Zheng Y (2020) Effect of enhanced recovery after surgery for elderly patients with hemiarthroplasty for the treatment of femoral neck fracture. Natl Med J China 100(37):2903–2907. https://doi.org/10.3760/cma.j.cn112137-20200308-00647
Wang YC, Yu WZ (2019) Application of accelerated rehabilitation program for the treatment of intertrochanteric fracture of femur in the elderly. Zhongguo gu shang = China journal of orthopaedics and traumatology 32(9):837–841. https://doi.org/10.3969/j.issn.1003-0034.2019.09.013
Zhu WH, Yan YJ, Sun YJ, Fan ZX, Fang NK, Zhang YL et al (2021) Implementation of Enhanced Recovery After Surgery (ERAS) protocol for elderly patients receiving surgery for intertrochanteric fracture: a propensity score-matched analysis. J Orthop Surg Res. https://doi.org/10.1186/s13018-021-02599-9
Wang P, Wang Q, Kong C, Teng Z, Li ZG, Zhang ST et al (2020) Enhanced recovery after surgery (ERAS) program for elderly patients with short-level lumbar fusion. J Orthop Surg Res. https://doi.org/10.1186/s13018-020-01814-3
Cui P, Wang P, Kong C, Li XY, Wang SK, Wang JL et al (2022) Patients older than 75 years undergoing polysegmental lumbar fusion surgery can also benefit from enhanced recovery after surgery program. Clin Interv Aging 17:245–252. https://doi.org/10.2147/CIA.S353511
Wang W, Wang P, Kong C, Teng Z, Zhang S, Sun W et al (2022) Retrospective data analysis for enhanced recovery after surgery (ERAS) protocol for elderly patients with long-level lumbar fusion. World Neurosurg. https://doi.org/10.1016/j.wneu.2022.04.109
Zuo XH, Wang LB, He LZ, Li P, Zhou DD, Yang YP (2021) Enhanced recovery after surgery protocol accelerates recovery of lumbar disc herniation among elderly patients undergoing discectomy via promoting gastrointestinal function. Pain Res Manag. https://doi.org/10.1155/2021/3573460
Li Z-E, Lu S-B, Kong C, Sun W-Z, Wang P, Zhang S-T (2021) Comparative short-term outcomes of enhanced recovery after surgery (ERAS) program and non-ERAS traditional care in elderly patients undergoing lumbar arthrodesis: a retrospective study. BMC Musculoskelet Disord 22(1):1–10. https://doi.org/10.1186/s12891-021-04166-z
Ifrach J, Basu R, Joshi DS, Flanders TM, Ozturk AK, Malhotra NR et al (2020) Efficacy of an enhanced recovery after surgery (ERAS) pathway in elderly patients undergoing spine and peripheral nerve surgery. Clin Neurol Neurosurg 197:106115–106115. https://doi.org/10.1016/j.clineuro.2020.106115
Zhang J, Che J, Sun X, Ren W (2022) Clinical application of perioperative anaesthesia management based on enhanced recovery after surgery concept to elderly patients undergoing total knee replacement. Comput Intell Neurosci 2022:8039358. https://doi.org/10.1155/2022/8039358
Olsen MF, Bjerre E, Hansen MD, Hilden J, Landler NE, Tendal B et al (2017) Pain relief that matters to patients: systematic review of empirical studies assessing the minimum clinically important difference in acute pain. BMC Med 15(1):35. https://doi.org/10.1186/s12916-016-0775-3
Hansen RN, Pham A, Strassels SA, Balaban S, Wan GJ (2016) Comparative analysis of length of stay and inpatient costs for orthopedic surgery patients treated with IV acetaminophen and IV opioids vs. IV opioids alone for post-operative pain. Adv Ther 33(9):1635–1645. https://doi.org/10.1007/s12325-016-0368-8
Liu SY, Li C, Zhang PX (2021) Enhanced recovery after surgery for hip fractures: a systematic review and meta-analysis. Perioper Med (London, England) 10(1):31. https://doi.org/10.1186/s13741-021-00201-8
Patel MR, Jacob KC, Chavez FA, Parsons AW, Seetharaman M, Pawlowski H et al (2023) Impact of postoperative length of stay on patient-reported and clinical outcomes after anterior lumbar interbody fusion. Int J Spine Surg 17(2):205–214. https://doi.org/10.14444/8414
Sarpong NO, Boddapati V, Herndon CL, Shah RP, Cooper HJ, Geller JA (2019) Trends in length of stay and 30-day complications after total knee arthroplasty: an analysis from 2006 to 2016. J Arthroplasty 34(8):1575–1580. https://doi.org/10.1016/j.arth.2019.04.027
Collopy BT, Cade RJ, Cocks JR, Davis CA (1991) Comparison of length of stay after hernia repair in two Victorian hospitals Standards Sub-committee of the Victorian State Committee of the Royal Australasian College of Surgeons. Aust N Z J Surg 61(4):276–279. https://doi.org/10.1111/j.1445-2197.1991.tb00211.x
Sinclair ST, Klika AK, Jin Y, Higuera CA, Piuzzi NS (2022) The impact of surgeon variability on patient-reported outcome measures, length of stay, discharge disposition, and 90-day readmission in TKA. J Bone Joint Surg Am 104(22):2016–2025. https://doi.org/10.2106/jbjs.21.01339
Henkelmann R, Theopold J, Kitsche J, Link PV, Mende M, Hepp P (2022) Comorbidities, substance abuse, weight and age are independent risk factors for postoperative complications following operation for proximal humerus fractures: a retrospective analysis of 1109 patients. Arch Orthop Trauma Surg 142(10):2701–2709. https://doi.org/10.1007/s00402-021-04022-8
Lee GC, Hodin RA (2019) Applying enhanced recovery pathways to unique patient populations. Clin Colon Rectal Surg 32(2):134–137. https://doi.org/10.1055/s-0038-1676479
Residori L, Bortolami O, Di Francesco V (2023) Hypoalbuminemia increases complications in elderly patients operated for hip fracture. Aging Clin Exp Res. https://doi.org/10.1007/s40520-023-02385-z
Tan JKH, Ang JJ, Chan DKH (2021) Enhanced recovery program versus conventional care after colorectal surgery in the geriatric population: a systematic review and meta-analysis. Surg Endosc 35(6):3166–3174. https://doi.org/10.1007/s00464-020-07673-7
Fagard K, Wolthuis A, D’Hoore A, Verhaegen M, Tournoy J, Flamaing J et al (2019) A systematic review of the intervention components, adherence and outcomes of enhanced recovery programmes in older patients undergoing elective colorectal surgery. BMC Geriatr 19(1):1–16. https://doi.org/10.1186/s12877-019-1158-3
Cusack B, Buggy DJ (2020) Anaesthesia, analgesia, and the surgical stress response. BJA Educ 20(9):321–328. https://doi.org/10.1016/j.bjae.2020.04.006
Li ZE, Lu SB, Kong C, Sun WZ, Wang P, Zhang ST (2020) Impact of compliance with an enhanced recovery after surgery program on the outcomes among elderly patients undergoing lumbar fusion surgery. Clin Interv Aging 15:2423–2430. https://doi.org/10.2147/cia.S286007
Acknowledgements
The authors thank all the clinicians and patients who have contributed to orthopedic researches.
Funding
This work was supported by [the Education Department of Liaoning Province, China] (Grant numbers [LJKZ1109]).
Author information
Authors and Affiliations
Contributions
PT: contributed to conceptualization, data curation, formal analysis, and writing—original draft. XZ: contributed to data curation and formal analysis. MH: contributed to conceptualization, methodology and supervision. BZ: contributed to conceptualization, supervision, and writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
None required.
Informed consent
None required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tan, P., Huo, M., Zhou, X. et al. The safety and effectiveness of enhanced recovery after surgery (ERAS) in older patients undergoing orthopedic surgery: a systematic review and meta-analysis. Arch Orthop Trauma Surg 143, 6535–6545 (2023). https://doi.org/10.1007/s00402-023-04963-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04963-2