Abstract
Introduction
The purpose of this study was to compare the distal femur morphology in different age and gender groups using the Citak classification.
Materials and methods
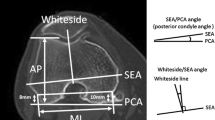
All patients who had standard knee anteroposterior radiographs between 2010 and 2020 were retrospectively reviewed using the electronic patient database. Patients were divided into three age groups as follows: young adults (Group I, younger than 50 years), middle-aged adults (Group II, ranging from age 51 to 73 years), and elderly (Group III, more than 74 years). From each age group, 80 patients were randomly selected with an equal number of gender (40 males/40 females). An age-stratified selection was applied to obtain the best sample that represents the selected age groups. Patients younger than 18 years of age, history of previous fracture or surgical procedure, those with fixation implants or prosthesis, and abnormalities of the lower limb, such as a congenital deformity, were excluded from the study. All measurements were performed by an experienced orthopedic surgeon familiar with the Citak classification. All measured variables were compared between age and gender groups.
Results
There were 240 patients (120 male and 120 female) with a mean age of 59.6 ± 20.4 (range 18–95). The distal femur morphology index was similar (p:0.811), and the morphological types were equally distributed among age groups (p:0.819). Furthermore, there was no significant difference between genders on the measured variables (p > 0.05 for all variables). Citak classification types were similarly distributed between the genders (p:0.153). No correlation was found between age and the Citak index in either gender (p:0.967 and p:0.633, respectively).
Conclusions
Distal femoral morphology classified by the Citak index is not age and gender dependent. Type C, which has a wider diaphyseal diameter, and is supposed to be more common in elderly subjects, was equally distributed in all age groups.
Level of evidence
Level IV.
Retrospective case series.



Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TKA :
-
Total knee arthroplasty
References
Maslaris A, Tsiridis E, Schoeneberg C et al (2022) Does stem profile have an impact on the failure patterns in revision total knee arthroplasty? Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04683-z
Innocenti B, Bori E, Pianigiani S (2022) Biomechanical analysis of the use of stems in revision total knee arthroplasty. Bioengineering. https://doi.org/10.3390/bioengineering9060259
Lee SH, Shih HN, Chang CH et al (2020) Influence of extension stem length and diameter on clinical and radiographic outcomes of revision total knee arthroplasty. BMC Musculoskelet Disord 21:1–10. https://doi.org/10.1186/s12891-019-3030-1
Levent A, Suero E, Gehrke T, Citak M (2021) Risk factors for aseptic loosening after total knee: a case-control study. J Bone Jt Surg 103:517–523
Citak M, Levent A, Suero EM et al (2022) A novel radiological classification system of the distal femur. Arch Orthop Trauma Surg 142:315–322. https://doi.org/10.1007/s00402-021-03828-w
Akkaya M, Simsek ME, Akcaalan S et al (2021) Validity of the novel radiological classification system of the distal femur. Z Orthop Unfall. https://doi.org/10.1055/a-1685-0955
Lawrence D, Dorr MD, Faugere Marie-Claude, Mackel Audley M, Gruen Thomas A, Bognar Benedek, Hartmut H, Malluche M (1993) Structural and cellular assessment of bone quality of proximal femur. Bone 3:231–242
Ahlborg HG, Johnell O, Karlsson MK (2004) An age-related medullary expansion can have implications for the long-term fixation of hip prostheses. Acta Orthop Scand 75:154–159. https://doi.org/10.1080/00016470412331294405
Keshawarz NM, Recker RR (1984) Expansion of the medullary cavity at the expense of cortex in postmenopausal osteoporosis. Metab Bone Dis Relat Res 5:223–228. https://doi.org/10.1016/0221-8747(84)90063-8
Salari N, Darvishi N, Bartina Y et al (2021) Global prevalence of osteoporosis among the world older adults: a comprehensive systematic review and meta-analysis. J Orthop Surg Res 16:1–13. https://doi.org/10.1186/s13018-021-02821-8
Hendrickx G, Boudin E, Van Hul W (2015) A look behind the scenes: The risk and pathogenesis of primary osteoporosis. Nat Rev Rheumatol 11:462–474. https://doi.org/10.1038/nrrheum.2015.48
Lanham-New SA (2008) Importance of calcium, vitamin D and vitamin K for osteoporosis prevention and treatment. Proc Nutr Soc 67:163–176. https://doi.org/10.1017/S0029665108007003
Santos L, Elliott-Sale KJ, Sale C (2017) Exercise and bone health across the lifespan. Biogerontology 18:931–946. https://doi.org/10.1007/s10522-017-9732-6
Tingart MJ, Apreleva M, von Stechow D et al (2003) The cortical thickness of the proximal humeral diaphysis predicts bone mineral density of the proximal humerus. J Bone Jt Surg Ser B 85:611–617. https://doi.org/10.1302/0301-620X.85B4.12843
Nguyen BNT, Hoshino H, Togawa D, Matsuyama Y (2018) Cortical thickness index of the proximal femur: A radiographic parameter for preliminary assessment of bone mineral density and osteoporosis status in the age 50 years and over population. CiOS Clin Orthop Surg 10:149–156. https://doi.org/10.4055/cios.2018.10.2.149
Stambough JB, Mason JB, Riesgo AM, Fehring TK (2018) Tapered modular fluted titanium stems for femoral fixation in revision total knee arthroplasty. Arthroplast Today 4:3–9. https://doi.org/10.1016/j.artd.2017.03.006
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37:691–697. https://doi.org/10.1016/j.injury.2006.04.130
Myers P, Laboe P, Johnson KJ et al (2018) Patient mortality in geriatric distal femur fractures. J Orthop Trauma 32:111–115. https://doi.org/10.1097/BOT.0000000000001078
Canton G, Giraldi G, Dussi M, et al (2019) Osteoporotic distal femur fractures in the elderly: Peculiarities and treatment strategies. Acta Biomed 90:25–32. https://doi.org/10.23750/abm.v90i12-S.8958
Acknowledgements
None.
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
M. F. Dasci: writing, data collection, editing, analysis. O. Kose: writing, data collection, statistics. M. Budin: data collection, analysis. S. Kara: analysis, statistics. T. Gerhke: supervision, proofreading. M. Citak: supervision, proofreading, editing. All authors contributed to the study conception and design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
M.C. has received funding from W. Link & Co KG outside the submitted work. T.G. has received funding from W. Link & Co KG, Zimmer Biomet Inc., Heraeus and from Ceramtec Co. outside the submitted work.
Ethical committee approval
Ethical approval was performed and has following number: 2022-300267-WF.
Consent to participate
Consent to participate is given.
Consent to publish
Consent to publish is given.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dasci, M.F., Kose, O., Budin, M. et al. Is the Citak classification of distal femur morphology age and gender dependent?. Arch Orthop Trauma Surg 143, 6773–6779 (2023). https://doi.org/10.1007/s00402-023-04959-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04959-y