Abstract
Introduction
Optimized health system approaches to improving guideline-congruent care require evaluation of multilevel factors associated with prescribing practices and outcomes after total knee and hip arthroplasty.
Materials and methods
Electronic health data from patients who underwent a total knee or hip arthroplasty between January 2016–January 2020 in the Military Health System Data were retrospectively analyzed. A generalized linear mixed-effects model (GLMM) examined the relationship between fixed covariates, random effects, and the primary outcome (30-day opioid prescription refill).
Results
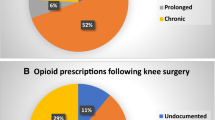
In the sample (N = 9151, 65% knee, 35% hip), the median discharge morphine equivalent dose was 660 mg [450, 892] and varied across hospitals and several factors (e.g., joint, race and ethnicity, mental and chronic pain conditions, etc.). Probability of an opioid refill was higher in patients who underwent total knee arthroplasty, were white, had a chronic pain or mental health condition, had a lower age, and received a presurgical opioid prescription (all p < 0.01). Sex assigned in the medical record, hospital duration, discharge non-opioid prescription receipt, discharge morphine equivalent dose, and receipt of an opioid-only discharge prescription were not significantly associated with opioid refill.
Conclusion
In the present study, several patient-, care-, and hospital-level factors were associated with an increased probability of an opioid prescription refill within 30 days after arthroplasty. Future work is needed to identify optimal approaches to reduce unwarranted and inequitable healthcare variation within a patient-centered framework.


Similar content being viewed by others
Data availability
All data generated or analyzed in this study are not included in this published article. The data is sourced from the US Department of Defense and cannot be made available directly to the public or individual researchers by the authors. Any request for data would need to go through the appropriate procedures (e.g., data sharing agreements) and authorities (Defense Health Agency).
References
Agency for Healthcare Research and Quality (2021) HCUP Fast Stats: 2018 U.S. National Inpatient Stays(ed)^(eds) Healthcare Cost and Utilization Project (HCUP), Rockville, MD.
Amen TB, Varady NH, Rajaee S, Chen AF (2020) Persistent racial disparities in utilization rates and perioperative metrics in total joint arthroplasty in the US: a comprehensive analysis of trends from 2006 to 2015. JBJS 102(9):811–820
Bates D, Mächler M, Bolker B, Walker S (2014) Fitting linear mixed-effects models using lme4. arXiv preprint arXiv:1406.5823. Accessed 22 Apr 2022
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 468(1):57–63
Brichetto G, Monti Bragadin M, Fiorini S et al (2020) The hidden information in patient-reported outcomes and clinician-assessed outcomes: multiple sclerosis as a proof of concept of a machine learning approach. Neurol Sci 41(2):459–462
Brummett CM, Waljee JF, Goesling J et al (2017) New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg 152(6):e170504
Buys MJ, Bayless K, Romesser J et al (2020) Opioid use among veterans undergoing major joint surgery managed by a multidisciplinary transitional pain service. Reg Anesth Pain Med 45(11):847–852
Chen EY, Lasky R, Dotterweich WA, Niu R, Tybor DJ, Smith EL (2019) Chronic prescription opioid use before and after total hip and knee arthroplasty in patients younger than 65 years. J Arthroplasty 34(10):2319–2323
Chou R, Gordon DB, de Leon-Casasola OA et al (2016) Management of postoperative pain: a clinical practice guideline from the American pain society, the American society of regional anesthesia and pain medicine, and the American society of anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. J Pain 17(2):131–157
Chun DS, Leonard AK, Enchill Z, Suleiman LI (2021) Racial disparities in total joint arthroplasty. Curr Rev Musculoskelet Med 14(6):434–440
Dover DC, Belon AP (2019) The health equity measurement framework: a comprehensive model to measure social inequities in health. Int J Equity Health 18(1):36
Dowell D, Haegerich TM, Chou R (2016) CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA 315(15):1624–1645
Grobaty L, Lajam C, Hutzler L (2020) Impact of value-based reimbursement on health-care disparities for total joint arthroplasty candidates. JBJS Rev 8(11):e2000073
Hansen CA, Inacio MCS, Pratt NL, Roughead EE, Graves SE (2017) Chronic use of opioids before and after total knee arthroplasty: a retrospective cohort study. J Arthroplasty 32(3):811-817.e811
Hoffman KM, Trawalter S, Axt JR, Oliver MN (2016) Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci USA 113(16):4296–4301
Kassambara A (2023) ggpubr: ‘ggplot2’ Based Publication Ready Plots. R package version 0.6.0. https://rpkgs.datanovia.com/ggpubr/. Accessed 1 Mar 2023
Kopp SL, Børglum J, Buvanendran A et al (2017) Anesthesia and analgesia practice pathway options for total knee arthroplasty: an evidence-based review by the american and european societies of regional anesthesia and pain medicine. Reg Anesth Pain Med 42(6):683–697
Kugelman DN, Mahure SA, Feng JE, Rozell JC, Schwarzkopf R, Long WJ (2021) Total knee arthroplasty is associated with greater immediate post-surgical pain and opioid use than total hip arthroplasty. Arch Orthop Trauma Surg. 142(12):3575–3580
Lewis GN, Rice DA, McNair PJ, Kluger M (2015) Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth. 114(4):551–561
Lindner M, Nosseir O, Keller-Pliessnig A, Teigelack P, Teufel M, Tagay S (2018) Psychosocial predictors for outcome after total joint arthroplasty: a prospective comparison of hip and knee arthroplasty. BMC Musculoskelet Disord 19(1):159–159
Ludecke D (2018) ggeffects: tidy data frames of marginal effects from regression models. J Open Sourc Soft 3(26):772
Namba RS, Singh A, Paxton EW, Inacio MCS (2018) Patient factors associated with prolonged postoperative opioid use after total knee arthroplasty. J Arthroplasty 33(8):2449–2454
Neuprez A, Neuprez AH, Kaux J-F et al (2017) Early clinically relevant improvement in quality of life and clinical outcomes 1 year postsurgery in patients with knee and hip joint arthroplasties. Cartilage 9(2):127–139
Nguyen L-CL, Sing DC, Bozic KJ (2016) Preoperative reduction of opioid use before total joint arthroplasty. J Arthroplasty 31(9):282–287
Nouraee CM, McGaver RS, Schaefer JJ et al (2022) Opioid-prescribing practices between total knee and hip arthroplasty in an outpatient versus inpatient setting. J Healthc Qual. 44(2):95–102
Novikov D, Cizmic Z, Feng JE, Iorio R, Meftah M (2018) The historical development of value-based care: how we got here. JBJS 100(22):e144
Politzer CS, Kildow BJ, Goltz DE, Green CL, Bolognesi MP, Seyler TM (2018) Trends in opioid utilization before and after total knee arthroplasty. J Arthroplasty. 33(7s):S147-153.e141
Pryymachenko Y, Wilson RA, Abbott JH, Dowsey MM, Choong PFM (2020) Risk factors for chronic opioid use following hip and knee arthroplasty: evidence from new Zealand population data. J Arthroplasty 35(11):3099-3107.e3014
Ripollés-Melchor J, Abad-Motos A, Díez-Remesal Y et al (2020) association between use of enhanced recovery after surgery protocol and postoperative complications in total hip and knee arthroplasty in the postoperative outcomes within enhanced recovery after surgery protocol in elective total hip and knee arthroplasty study (POWER2). JAMA Surg 155(4):e196024
Roebke AJ, Via GG, Everhart JS et al (2020) Inpatient and outpatient opioid requirements after total joint replacement are strongly influenced by patient and surgical factors. Bone Jt Open 1(7):398–404
Ruddell JH, Reid DBC, Shah KN et al (2021) Larger initial opioid prescriptions following total joint arthroplasty are associated with greater risk of prolonged use. J Bone Joint Surg 103(2):106–114 (American volume)
Sabatino MJ, Kunkel ST, Ramkumar DB, Keeney BJ, Jevsevar DS (2018) Excess opioid medication and variation in prescribing patterns following common orthopaedic procedures. J Bone Joint Surg 100(3):180–188 (American volume)
Samra R, Hankivsky O (2021) Adopting an intersectionality framework to address power and equity in medicine. The Lancet 397(10277):857–859
Shah A, Hayes CJ, Martin BC (2017) Characteristics of initial prescription episodes and likelihood of long-term opioid use—United States, 2006–2015. MMWR Morb Mortal Wkly Rep 66:265–269
Sheth DS, Ho N, Pio JR, Zill P, Tovar S, Namba RS (2020) Prolonged opioid use after primary total knee and total hip arthroplasty: prospective evaluation of risk factors and psychological profile for depression, pain catastrophizing, and aberrant drug-related behavior. J Arthroplasty 35(12):3535–3544
Soffin EM, Wilson LA, Liu J, Poeran J, Memtsoudis SG (2021) Association between sex and perioperative opioid prescribing for total joint arthroplasty: a retrospective population-based study. Br J Anaesth 126(6):1217–1225
Sorel J, Veltman E, Honig A, Poolman R (2019) The influence of preoperative psychological distress on pain and function after total knee arthroplasty: a systematic review and meta-analysis. Bone Joint J 101(1):7–14
Subirana I, Sanz H, Vila J (2014) Building bivariate tables: the comparegroups package for R. J Stat Softw 1(12):2014
Traven SA, Brinton DL, Woolf SK, Leddy LR, Gottschalk MB, Slone HS (2021) Notable variability in opioid-prescribing practices after common orthopaedic procedures. J Am Acad Orthop Surg. 29(5):219–226
Vaz KM, Huang PS, Copp SN (2019) Standardized opioid prescription protocol reduces opioid consumption after total joint arthroplasty. J Am Acad Orthop Surg Glob Res Rev. 3(12):e19.00163
Whale CS, Henningsen JD, Huff S, Schneider AD, Hijji FY, Froehle AW (2020) Effects of the Ohio opioid prescribing guidelines on total joint arthroplasty postsurgical prescribing and refilling behavior of surgeons and patients. J Arthroplasty 35(9):2397–2404
Wickham H (2016) ggplot2: elegent graphics for data analysis. Springer-Verlag, New York, New York
Wilson Y, White A, Jefferson A, Danis M (2019) Intersectionality in clinical medicine: the need for a conceptual framework. Am J Bioeth 19(2):8–19
Woo A, Lechner B, Fu T et al (2015) Cut points for mild, moderate, and severe pain among cancer and non-cancer patients: a literature review. Ann Palliat Med 4(4):176–183
Young JC, Dasgupta N, Chidgey BA, Jonsson Funk M (2021) Postsurgical opioid prescriptions and risk of long-term use: an observational cohort study across the United States. Ann Surg 273(4):743–750
Zalon ML (2014) Mild, moderate, and severe pain in patients recovering from major abdominal surgery. Pain Manag nursing 15(2):e1–e12
Funding
Funding for this project was provided by the Uniformed Services University through Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc. under Cooperative Agreement #HU00011920042.
Author information
Authors and Affiliations
Contributions
All authors contributed to the present manuscript, to include contributing to the (1) conceptualization, (2) interpretation of analytic results, (3) writing of the first draft, (4) and editing of the first draft. Krista Highland provided supervision; Krista Highland and Alexander Velosky contributed to the methodology and formal analysis and investigation.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The views expressed are solely those of the authors and do not reflect the official policy or position of the Uniformed Services University, US Army, US Navy, US Air Force, the Department of Defense, the US Government, or the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Highland, K.B., Sowa, H.A., Herrera, G.F. et al. Post-total joint arthroplasty opioid prescribing practices vary widely and are not associated with opioid refill: an observational cohort study. Arch Orthop Trauma Surg 143, 5539–5548 (2023). https://doi.org/10.1007/s00402-023-04853-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04853-7