Abstract
Objective
Posterior cruciate-stabilized (PS) and ultracongruent (UC) inserts are used during total knee arthroplasty (TKA), but superiority in gaining postoperative knee flexion and functionality remains contested. Therefore, this study compared postoperative outcomes between PS and UC inserts.
Methods
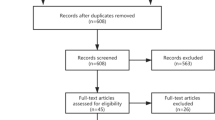
A retrospective review evaluated unilateral or bilateral TKAs with PS or UC inserts from August 2011 to March 2020. Nonparametric statistics were performed to evaluate differences in patient demographics, pre- and postknee flexion and Knee Society Knee (KSS-K) and Function Score (KSS-F). Univariate and multivariable regressions were performed to evaluate the influence on postoperative knee flexion ≥ 120°, presented as odds ratios (OR) and 95% confidence intervals (CI).
Results
Patient demographics were not significantly different between the 577 PS and 399 UC knees evaluated. Postoperatively, a larger proportion of UC knees demonstrated knee flexion < 120° (36.0% vs. 18.6%, p < 0.001) and lower KSS-K (91.0 ± 8.7 vs. 91.6 ± 10.3, p < 0.001) and KSS-F (76.8 ± 21.6 vs. 79.9 ± 21.6, p = 0.007) than the PS group. The PS group had greater improvement in flexion angle (4.9° ± 14.9° vs. 1.0° ± 15.6°, p < 0.001) and KSS-F (27.3 ± 23.3 vs. 23.1 ± 25.3, p = 0.007) as compared to that of UC patients. Patients with preoperative flexion < 120° (OR 2.787, CI 2.066–3.761; p < 0.001), higher body mass index (OR 1.033, CI 1.006–1.061; p = 0.017) and UC insert (OR 2.461, CI 1.832–3.307; p < 0.001) were less likely to achieve flexion ≥ 120°.
Conclusion
Favorable clinical and functional outcomes were noted in the PS group as compared to UC inserts in TKA. The greater improvement in overall knee flexion may suggest the PS insert may be especially appropriate for patients with lower preoperative range of motion.
Level of evidence
III, retrospective comparative study.
Similar content being viewed by others
Data availability
Data for this study is kept in a secure repository and can be accessed with permission for appropriate requests.
References
(2020) American Joint Replacement Registry Annual Report
Fantozzi S, Catani F, Ensini A et al (2006) Femoral rollback of cruciate-retaining and posterior-stabilized total knee replacements: in vivo fluoroscopic analysis during activities of daily living. J Orthop Res 24:2222–2229. https://doi.org/10.1002/jor.20306
Maruyama S, Yoshiya S, Matsui N et al (2004) Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty 19:349–353. https://doi.org/10.1016/j.arth.2003.09.010
Kumar N, Yadav C, Raj R, Yadav S (2015) Fracture of the polyethylene tibial post in a posterior stabilized knee prosthesis: a case report and review of literature. J Orthop 12:160–163. https://doi.org/10.1016/j.jor.2015.01.002
Bal BS, Greenberg D, Li S et al (2008) Tibial post failures in a condylar posterior cruciate substituting total knee arthroplasty. J Arthroplasty 23:650–655. https://doi.org/10.1016/j.arth.2007.08.002
Diamond OJ, Howard L, Masri B (2018) Five cases of tibial post fracture in posterior stabilized total knee arthroplasty using Prolong highly cross-linked polyethylene. Knee 25:657–662. https://doi.org/10.1016/j.knee.2018.05.005
Chiu Y-S, Chen W-M, Huang C-K et al (2004) Fracture of the polyethylene tibial post in a NexGen posterior-stabilized knee prosthesis. J Arthroplasty 19:1045–1049. https://doi.org/10.1016/j.arth.2004.04.013
Clarke HD, Math KR, Scuderi GR (2004) Polyethylene post failure in posterior stabilized total knee arthroplasty1. J Arthroplasty 19:652–657. https://doi.org/10.1016/j.arth.2004.02.026
Sherman WF, Mansour A, Sanchez FL, Wu VJ (2020) Increased intercondylar femoral box cut-to-femur size ratio during posterior-stabilized total knee arthroplasty increases risk for intraoperative fracture. Arthroplasty Today 6:180–185. https://doi.org/10.1016/j.artd.2020.03.014
Lombardi AV, Mallory TH, Waterman RA, Eberle RW (1995) Intercondylar distal femoral fracture: an unreported complication of posterior-stabilized total knee arthroplasty. J Arthroplasty 10:643–650. https://doi.org/10.1016/S0883-5403(05)80209-8
Mak Y-F, Lee Q-J, Chang W-YE, Wong Y-C (2020) Intraoperative femoral condyle fracture in primary total knee arthroplasty—a case–control study in Asian population. Knee Surg Relat Res 32:31. https://doi.org/10.1186/s43019-020-00043-6
Furman BD, Lipman J, Kligman M et al (2008) Tibial post wear in posterior-stabilized knee replacements is design-dependent. Clin Orthop Relat Res 466:2650–2655. https://doi.org/10.1007/s11999-008-0422-1
Renson D, Lenaerts W, Feyen J (2019) Nontraumatic fracture of the polyethylene tibial post in a bi-cruciate stabilized total knee prosthesis. Arthroplasty Today 5:284–287. https://doi.org/10.1016/j.artd.2019.06.001
Hendel D, Garti A, Weisbort M (2003) Fracture of the central polyethylene tibial spine in posterior stabilized total knee arthroplasty. J Arthroplasty 18:672–674. https://doi.org/10.1016/s0883-5403(03)00192-x
Dolan M, Kelly N, LeFloch S et al (2010) Tibial Post Wear In Posterior-Stabilized Knee Replacements: A Comparison Of Three Contemporary Designs. J Arthroplasty 25:e39. https://doi.org/10.1016/j.arth.2010.01.047
Puloski SK, McCalden RW, MacDonald SJ et al (2001) Tibial post wear in posterior stabilized total knee arthroplasty. An unrecognized source of polyethylene debris. J Bone Jt Surg Am 83:390–397. https://doi.org/10.2106/00004623-200103000-00011
Mazzucchelli L, Deledda D, Rosso F et al (2016) Cruciate retaining and cruciate substituting ultra-congruent insert. Ann Transl Med. https://doi.org/10.3978/j.issn.2305-5839.2015.12.52
Volkmar AJ, Elrod R, Vickery JW et al (2022) Cruciate substituting implants in primary total knee arthroplasty. Adv Orthop 2022:2676715. https://doi.org/10.1155/2022/2676715
Dalton P, Holder C, Rainbird S, Lewis PL (2021) Survivorship comparisons of ultracongruent, cruciate-retaining and posterior-stabilized tibial inserts using a single knee system design: results from the Australian Orthopedic Association National Joint Replacement Registry. J Arthroplasty. https://doi.org/10.1016/j.arth.2021.11.001
Spekenbrink-Spooren A, Van Steenbergen LN, Denissen GAW et al (2018) Higher mid-term revision rates of posterior stabilized compared with cruciate retaining total knee arthroplasties: 133,841 cemented arthroplasties for osteoarthritis in the Netherlands in 2007–2016. Acta Orthop 89:640–645. https://doi.org/10.1080/17453674.2018.1518570
Yoon J-R, Yang J-H (2018) Satisfactory short-term results of navigation-assisted gap-balancing total knee arthroplasty using ultracongruent insert. J Arthroplasty 33:723–728. https://doi.org/10.1016/j.arth.2017.09.049
Chavoix J-B (2013) Functionality and safety of an ultra-congruent rotating platform knee prosthesis at 5.6 years: more than 5-year follow-up of the e.motion UC-TKA. Open Orthop J. https://doi.org/10.2174/1874325001307010152
Bae J-H, Yoon J-R, Sung J-H, Shin Y-S (2018) Posterior-stabilized inserts are preferable to cruciate-substituting ultracongruent inserts due to more favourable kinematics and stability. Knee Surg Sports Traumatol Arthrosc 26:3300–3310. https://doi.org/10.1007/s00167-018-4872-z
Fritzsche H, Beyer F, Postler A, Lützner J (2018) Different intraoperative kinematics, stability, and range of motion between cruciate-substituting ultracongruent and posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26:1465–1470. https://doi.org/10.1007/s00167-017-4427-8
Kim TW, Lee SM, Seong SC et al (2016) Different intraoperative kinematics with comparable clinical outcomes of ultracongruent and posterior stabilized mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:3036–3043. https://doi.org/10.1007/s00167-014-3489-0
Machhindra MV, Kang JY, Kang YG et al (2015) Functional outcomes of a new mobile-bearing ultra-congruent TKA system: comparison with the posterior stabilized system. J Arthroplasty 30:2137–2142. https://doi.org/10.1016/j.arth.2015.06.011
Lee S-S, Yeom J, Lee D-H, Moon Y-W (2020) Similar outcomes between ultracongruent and posterior-stabilized insert in total knee arthroplasty: a propensity score-matched analysis. J Orthop Surg (Hong Kong) 28:2309499019893515. https://doi.org/10.1177/2309499019893515
Lützner J, Beyer F, Dexel J et al (2017) No difference in range of motion between ultracongruent and posterior stabilized design in total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 25:3515–3521. https://doi.org/10.1007/s00167-016-4331-7
Parsley BS, Bertolusso R, Harrington M et al (2010) Influence of gender on age of treatment with TKA and functional outcome. Clin Orthop Relat Res 468:1759–1764. https://doi.org/10.1007/s11999-010-1348-y
Andrews SN, Beeler DM, Parke EA et al (2019) Fixed distal femoral cut of 6° valgus in total knee arthroplasty: a radiographic review of 788 consecutive cases. J Arthroplasty 34:755–759. https://doi.org/10.1016/j.arth.2018.12.013
Blonna D, Zarkadas PC, Fitzsimmons JS, O’Driscoll SW (2012) Accuracy and inter-observer reliability of visual estimation compared to clinical goniometry of the elbow. Knee Surg Sports Traumatol Arthrosc 20:1378–1385. https://doi.org/10.1007/s00167-011-1720-9
Babazadeh S, Dowsey MM, Stone JD, Choong PFM (2012) The accuracy of retrospectively measured range of motion in knee arthroplasty. Acta Orthop Belg 78:751–756
Russo RR, Burn MB, Ismaily SK et al (2017) Is digital photography an accurate and precise method for measuring range of motion of the hip and knee? J Exp Orthop 4:29. https://doi.org/10.1186/s40634-017-0103-7
Jiang C, Liu Z, Wang Y et al (2016) Posterior cruciate ligament retention versus posterior stabilization for total knee arthroplasty: a meta-analysis. PLoS One 11:e0147865. https://doi.org/10.1371/journal.pone.0147865
Massin P, Boyer P, Sabourin M (2012) Less femorotibial rotation and AP translation in deep-dished total knee arthroplasty. An intraoperative kinematic study using navigation. Knee Surg Sports Traumatol Arthrosc 20:1714–1719. https://doi.org/10.1007/s00167-011-1740-5
Gandhi R, de Beer J, Leone J et al (2006) Predictive risk factors for stiff knees in total knee arthroplasty. J Arthroplasty 21:46–52. https://doi.org/10.1016/j.arth.2005.06.004
Ritter MA, Berend ME, Harty LD et al (2004) Predicting range of motion after revision total knee arthroplasty: clustering and log-linear regression analyses. J Arthroplasty 19:338–343. https://doi.org/10.1016/j.arth.2003.11.001
Sahu NK, Patnaik S, Nanda S, Jain M (2019) Variables determining the postoperative knee range of motion following cruciate-substituting total knee replacement: a prospective study. Cureus. https://doi.org/10.7759/cureus.5501
Farahini H, Moghtadaei M, Bagheri A, Akbarian E (2012) Factors influencing range of motion after total knee arthroplasty. Iran Red Crescent Med J 14:417–421
Bade MJ, Kittelson JM, Kohrt WM, Stevens-Lapsley JE (2014) Predicting functional performance and range of motion outcomes after total knee arthroplasty. Am J Phys Med Rehabil 93:579–585. https://doi.org/10.1097/PHM.0000000000000065
Maniar RN, Maniar PR, Singhi T, Gangaraju BK (2018) WHO class of obesity influences functional recovery post-TKA. Clin Orthop Surg 10:26–32. https://doi.org/10.4055/cios.2018.10.1.26
Naziri Q, Issa K, Malkani AL et al (2013) Bariatric orthopaedics: total knee arthroplasty in super-obese patients (BMI > 50 kg/m2). survivorship and complications. Clin Orthop Relat Res 471:3523–3530. https://doi.org/10.1007/s11999-013-3154-9
Gaillard R, Gaillard T, Denjean S, Lustig S (2017) No influence of obesity on survival of cementless, posterior-stabilised, rotating-platform implants. Arch Orthop Trauma Surg 137:1743–1750. https://doi.org/10.1007/s00402-017-2801-0
Kim MS, Koh IJ, Kim CK et al (2021) Comparison of joint perception between posterior-stabilized and ultracongruent total knee arthroplasty in the same patient. JBJS 103:44–52. https://doi.org/10.2106/JBJS.20.00279
Akti S, Karakus D, Sezgin EA, Cankaya D (2020) No differences in clinical outcomes or isokinetic performance between cruciate-substituting ultra-congruent and posterior stabilized total knee arthroplasties: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06275-z
Yacovelli S, Grau LC, Hozack WJ, Courtney PM (2021) Functional outcomes are comparable between posterior stabilized and cruciate-substituting total knee arthroplasty designs at short-term follow-up. J Arthroplasty 36:986–990. https://doi.org/10.1016/j.arth.2020.09.008
Carlson BJ, Jones BK, Scott DF (2022) A prospective comparison of total knee arthroplasty using ultra-congruent, condylar-stabilizing, and posterior-stabilized devices implanted with kinematic alignment: better 2-year outcomes with ultra-congruent. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07206-w
Lützner J, Beyer F, Lützner C et al (2021) Ultracongruent insert design is a safe alternative to posterior cruciate-substituting total knee arthroplasty: 5-year results of a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06545-4
Matsuda S, Whiteside LA, White SE, McCarthy DS (1997) Knee kinematics of posterior cruciate ligament sacrificed total knee arthroplasty. Clin Orthop Relat Res 341:257–266
Galea VP, Botros MA, Madanat R et al (2019) Promising early outcomes of a novel anatomic knee system. Knee Surg Sports Traumatol Arthrosc 27:1067–1074. https://doi.org/10.1007/s00167-018-5248-0
Mathijssen NMC, Verburg H, London NJ et al (2019) Patient reported outcomes and implant survivorship after Total knee arthroplasty with the persona knee implant system: two year follow up. BMC Musculoskelet Disord 20:97. https://doi.org/10.1186/s12891-019-2470-y
Christensson A, Tveit M, Kesteris U, Flivik G (2022) Similar migration for medial congruent and cruciate-retaining tibial components in an anatomic TKA system: a randomized controlled trial of 60 patients followed with RSA for 2 years. Acta Orthop 93:68–74. https://doi.org/10.1080/17453674.2021.1983709
Alesi D, Di Paolo S, Bragonzoni L et al (2022) No kinematical difference between ultra-congruent and medial-congruent total knee arthroplasty when implanted with mechanical alignment: an in vivo dynamic RSA study. Knee Surg Sports Traumatol Arthrosc 30:2975–2979. https://doi.org/10.1007/s00167-022-07033-z
Roberti di Sarsina T, Alesi D, Di Paolo S et al (2022) In vivo kinematic comparison between an ultra-congruent and a posterior-stabilized total knee arthroplasty design by RSA. Knee Surg Sports Traumatol Arthrosc 30:2753–2758. https://doi.org/10.1007/s00167-021-06629-1
Yokhana SS, Hamilton DA, Stine SA et al (2021) The prevalence of posterolateral tibial baseplate overhang: an anatomical CT study. J Orthop 23:259–263. https://doi.org/10.1016/j.jor.2021.02.002
Ma Y, Mizu-uchi H, Okazaki K et al (2018) Effects of tibial baseplate shape on rotational alignment in total knee arthroplasty: three-dimensional surgical simulation using osteoarthritis knees. Arch Orthop Trauma Surg 138:105–114. https://doi.org/10.1007/s00402-017-2828-2
Kocak UZ, Guran O, Kalkan S et al (2021) Assessing the knee flexion range of motion after total knee arthroplasty: technology versus senses. J Bodyw Mov Ther 28:547–551. https://doi.org/10.1016/j.jbmt.2021.09.011
Acknowledgements
The authors would like to thank Samantha N. Andrews Ph.D., ATC, for her contributions regarding statistical analysis and help with student mentoring and manuscript preparation.
Funding
This research received no specific grant from any funding agency in the public, commercial or non-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Ethical approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Hawai‘i Pacific Health Research Institute (local Western Institutional Review Board) approved this study.
Informed consent
This was a retrospective chart review and data collected were deidentified and presented as large scale, aggregate data. Therefore, no informed consent was obtained or required by the IRB.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Obana, K.K., Wong, K., Shimoda, B.T. et al. Favorable outcomes of posterior cruciate-stabilized inserts over ultracongruent inserts in total knee arthroplasty. Arch Orthop Trauma Surg 143, 5857–5865 (2023). https://doi.org/10.1007/s00402-023-04837-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04837-7