Abstract
Introduction
As recent analyses have indicated that low-volume hospitals experience higher rates of complications following total knee arthroplasty (TKA), it remains important to evaluate how area deprivation index (ADI) of hospitals impacts the quantity of TKA performed. Our analysis sought to evaluate how the ADI of orthopedic surgeon’s place of service influences TKA utilization.
Materials and methods
The Medicare Provider Utilization and Payment Data Public Use File (MPUP-PUF) was queried to identify claims between 2013 and 2019 associated with Healthcare Common Procedure Coding System (HCPCS) code 27447 (TKA). The MPUP-PUF file was linked with publicly available ADI information as well as information regarding each provider’s practice location. The Mann–Kendall trend test was used to analyze significant differences in TKA volume between ADI quintiles and differences in TKA volume overall between the years 2013 and 2019. An adjusted multivariable linear regression analysis was conducted to evaluate how ADI, and practice-specific characteristics, influenced TKA utilization volume.
Results
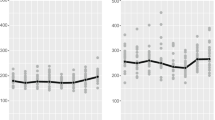
When isolating by ADI quintiles, no significant changes in TKA volume were demonstrated for Quintile 4 (Kendall’s τ = 0.524; p = 0.13) and Quintile 5 (Kendall’s τ = 0.524; p = 0.13) between 2013 and 2019. However, a significant increase in TKA volume over the study period was observed in Quintile 1 (Kendall’s τ = 0.714 p = 0.034), Quintile 2 (Kendall’s τ = 0.714 p = 0.034), and Quintile 3 (Kendall’s τ = 0.905 p = 0.007). The adjusted multivariable linear regression model demonstrated that each increase in ADI quintile was associated with significantly lower TKA utilization (β-estimate − 1.16; 95% CI − 2.04 to − 0.29; p = 0.009).
Conclusions
Our findings suggest that resource deprivation contributes to disparities in TKA utilization. With the ongoing recognition of how social and neighborhood-level deprivation may influence access to end-stage osteoarthritis care and related perioperative outcomes, the present study serves to encourage continued efforts at ensuring equity in orthopedic care.


Similar content being viewed by others
References
Kurtz S, Ong K, Lau E et al (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg Ser A. https://doi.org/10.2106/JBJS.F.00222
Sloan M, Premkumar A, Sheth NP (2018) Projected volume of primary total joint arthroplasty in the US, 2014 to 2030. J Bone Jt Surg 100:1455–1460. https://doi.org/10.2106/JBJS.17.01617
Courtney PM, Huddleston JI, Iorio R, Markel DC (2017) Socioeconomic risk adjustment models for reimbursement are necessary in primary total joint arthroplasty. J Arthroplast 32:1–5. https://doi.org/10.1016/J.ARTH.2016.06.050
Inneh IA, Clair AJ, Slover JD, Iorio R (2016) Disparities in discharge destination after lower extremity joint arthroplasty: analysis of 7924 patients in an urban setting. J Arthroplast 31:2700–2704. https://doi.org/10.1016/J.ARTH.2016.05.027
Keeney JA, Nam D, Johnson SR et al (2015) Socioeconomically disadvantaged CMS beneficiaries do not benefit from the readmission reduction initiatives. J Arthroplast 30:2082–2085. https://doi.org/10.1016/J.ARTH.2015.06.031
Lavernia CJ, Villa JM (2015) Does race affect outcomes in total joint arthroplasty? Clin Orthop Relat Res 473:3535–3541. https://doi.org/10.1007/S11999-015-4481-9
Rosenthal BD, Hulst JB, Moric M et al (2014) The effect of payer type on clinical outcomes in total knee arthroplasty. J Arthroplast 29:295–298. https://doi.org/10.1016/J.ARTH.2013.06.010
Rubenstein WJ, Harris AHS, Hwang KM et al (2020) Social determinants of health and patient-reported outcomes following total hip and knee arthroplasty in veterans. J Arthroplast 35:2357–2362. https://doi.org/10.1016/J.ARTH.2020.04.095
Thirukumaran CP, Cai X, Glance LG et al (2020) Geographic variation and disparities in total joint replacement use for medicare beneficiaries: 2009 to 2017. J Bone Jt Surg Am 102:2120–2128. https://doi.org/10.2106/JBJS.20.00246
Hinman A, Bozic KJ (2008) Impact of payer type on resource utilization, outcomes and access to care in total hip arthroplasty. J Arthroplast 23:9–14. https://doi.org/10.1016/J.ARTH.2008.05.010
Knighton AJ, Savitz L, Belnap T et al (2016) Introduction of an area deprivation index measuring patient socioeconomic status in an integrated health system: implications for population health. J Electron Health Data Methods 4:9
Neighborhood Atlas. https://www.neighborhoodatlas.medicine.wisc.edu. Accessed 23 Nov 2021
Cheng AL, McDuffie JV, Schuelke MJ et al (2022) How should we measure social deprivation in orthopaedic patients? Clin Orthop Relat Res. https://doi.org/10.1097/CORR.0000000000002044
Meza BC, Iacone D, Talwar D et al (2020) Socioeconomic deprivation and its adverse association with adolescent fracture care compliance. JBJS Open Access 5:e0064–e0064. https://doi.org/10.2106/JBJS.OA.19.00064
Jeschke E, Citak M, Günster C et al (2017) Are TKAs performed in high-volume hospitals less likely to undergo revision than TKAs performed in low-volume hospitals? Clin Orthop Relat Res 475:2669. https://doi.org/10.1007/S11999-017-5463-X
Brodeur PG, Kim KW, Modest JM et al (2022) Surgeon and facility volume are associated with postoperative complications after total knee arthroplasty. Arthroplast Today. https://doi.org/10.1016/J.ARTD.2021.11.017
Medicare Physician and Other Practitioners—by Provider and Service—Centers for Medicare and Medicaid Services Data. https://data.cms.gov/provider-summary-by-type-of-service/medicare-physician-other-practitioners/medicare-physician-other-practitioners-by-provider-and-service/data/2019. Accessed 23 Dec 2021
Medicare Physician and Other Practitioners—by Provider—Centers for Medicare and Medicaid Services Data. https://data.cms.gov/provider-summary-by-type-of-service/medicare-physician-other-practitioners/medicare-physician-other-practitioners-by-provider/data/2019#. Accessed 23 Dec 2021
Geocode and map spreadsheets in a snap—Geocodio. https://www.geocod.io/features/spreadsheet/. Accessed 23 Dec 2021
Office UCBPI Census Bureau Releases Comprehensive Analysis of Fast-Growing 90-and-Older Population—Aging Population—Newsroom—US Census Bureau
Kind AJH, Buckingham WR (2018) Making neighborhood-disadvantage metrics accessible—the neighborhood atlas. N Engl J Med 378:2456–2458. https://doi.org/10.1056/NEJMP1802313
Rahman M, Meyers DJ, Wright B (2020) Unintended consequences of observation stay use may disproportionately burden medicare beneficiaries in disadvantaged neighborhoods. Mayo Clin Proc 95:2589–2591. https://doi.org/10.1016/J.MAYOCP.2020.10.014
Powell WR, Buckingham WR, Larson JL et al (2020) Association of neighborhood-level disadvantage with Alzheimer disease neuropathology. JAMA Netw Open 3:e207559–e207559. https://doi.org/10.1001/JAMANETWORKOPEN.2020.7559
Mora J, Krepline AN, Aldakkak M et al (2021) Adjuvant therapy rates and overall survival in patients with localized pancreatic cancer from high Area Deprivation Index neighborhoods. Am J Surg 222:10–17. https://doi.org/10.1016/J.AMJSURG.2020.12.001
Inacio MCS, Paxton EW, Graves SE et al (2017) Projected increase in total knee arthroplasty in the United States—an alternative projection model. Osteoarthr Cartil 25:1797–1803. https://doi.org/10.1016/J.JOCA.2017.07.022
Singh JA, Yu S, Chen L, Cleveland JD (2019) Rates of total joint replacement in the united states: future projections to 2020–2040 using the national inpatient sample. J Rheumatol 46:1134–1140. https://doi.org/10.3899/JRHEUM.170990
Kugler CM, Goossen K, Rombey T et al (2021) Hospital volume-outcome relationship in total knee arthroplasty: a systematic review and dose-response meta-analysis. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/S00167-021-06692-8
Yu TH, Chou YY, Tung YC (2019) Should we pay attention to surgeon or hospital volume in total knee arthroplasty? Evidence from a nationwide population-based study. PLoS ONE. https://doi.org/10.1371/JOURNAL.PONE.0216667
Singh JA, Kwoh CK, Boudreau RM et al (2011) Hospital volume and surgical outcomes after elective hip/knee arthroplasty: a risk adjusted analysis of a large regional database. Arthritis Rheum 63:2531. https://doi.org/10.1002/ART.30390
Namba RS, Inacio MCS, Paxton EW (2013) Risk factors associated with deep surgical site infections after primary total knee arthroplasty: an analysis of 56,216 knees. J Bone Jt Surg Am 95:775–782. https://doi.org/10.2106/JBJS.L.00211
Clement N (2013) Patient factors that influence the outcome of total knee replacement: a critical review of the literature. OA Orthop. https://doi.org/10.13172/2052-9627-1-2-697
Brennan-Olsen S, Vogrin S, Holloway KL et al (2017) Geographic region, socioeconomic position and the utilisation of primary total joint replacement for hip or knee osteoarthritis across western Victoria: a cross-sectional multilevel study of the Australian Orthopaedic Association National Joint Replacement Registry. Arch Osteoporos. https://doi.org/10.1007/s11657-017-0396-2
Thomas L Health Care Facilities Are Leaving Poor City Neighborhoods. https://www.governing.com/news/headlines/health-care-facilities-are-leaving-poor-city-neighborhoods.html. Accessed 14 Apr 2022
Thomas L Poor Health | Special Report—Hospitals, doctors moving out of poor city neighborhoods to more affluent areas. https://archive.jsonline.com/news/health/hospitals-doctors-moving-out-of-poor-city-neighborhoods-to-more-affluent-areas-b99284882z1-262899701.html/. Accessed 14 Apr 2022
Garcis R Why are doctors and hospitals leaving neighborhoods that need healthcare the most? Lightspeed revenue cycle management. https://lightspeedrcm.com/uncategorized/why-are-doctors-and-hospitals-leaving-neighborhoods-that-need-healthcare-the-most/. Accessed 14 Apr 2022
Hawker GA, Wright JG, Glazier RH et al (2002) The effect of education and income on need and willingness to undergo total joint arthroplasty. Arthritis Rheum 46:3331–3339. https://doi.org/10.1002/ART.10682
Carmichael H, Tran B, Velopulos CG (2022) When more is less: urban disparities in access to surgical care by transportation means. Am J Surg 223:112–119. https://doi.org/10.1016/J.AMJSURG.2021.07.052
Hartnett DA, Brodeur PG, Kosinski LR et al (2022) Socioeconomic disparities in the utilization of total hip arthroplasty. J Arthroplast. https://doi.org/10.1016/J.ARTH.2021.10.021
Michel M, Bryère J, Maravic M, Marcelli C (2019) Knee replacement incidence and social deprivation: results from a French ecological study. Jt Bone Spine 86:637–641. https://doi.org/10.1016/j.jbspin.2019.03.004
Cooper RA, Cooper MA, McGinley EL et al (2012) Poverty, wealth, and health care utilization: a geographic assessment. J Urban Health 89:828. https://doi.org/10.1007/S11524-012-9689-3
Horwitz JR (2005) Market watch: Making profits and providing care: comparing nonprofit, for-profit, and government hospitals—discussion of the value of nonprofit hospital ownership must account for the differences in service offerings among hospital types. Health Aff 24:790–801. https://doi.org/10.1377/HLTHAFF.24.3.790
Funding
No funding was received for our analysis.
Author information
Authors and Affiliations
Contributions
VSW, AJA, AFK were involved in the study concept and design. VSW and AJA were involved in the acquisition of data and analysis of the data. VSW, AJA, AGK, RJB were involved in the drafting of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
A.F.K. reports the following disclosures: research support (Signature Orthopedics), paid presenter or speaker (DePuy Synthes and Zimmer Biomet), paid consultant (DePuy Synthes and Zimmer Biomet), stock or stock options (Zimmer Biomet, Johnson & Johnson, and Procter & Gamble), IP royalties (Innomed), and board or committee member (AAOS, AAHKS, and Anterior Hip Foundation). V.S.W, A.J.A., R.J.B, and A.G.K have nothing to disclose.
Ethical approval
Our analysis included de-identified information from a publicly available dataset and therefore, IRB approval was not required.
Informed consent
Our analysis included de-identified information from a publicly available dataset and therefore, patient consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, V.S., Acuña, A.J., Kim, A.G. et al. Impact of social disadvantage among total knee arthroplasty places of service on procedural volume: a nationwide Medicare analysis. Arch Orthop Trauma Surg 143, 4579–4585 (2023). https://doi.org/10.1007/s00402-022-04708-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04708-7