Abstract
Background
Reverse total shoulder arthroplasty (RTSA) can decrease shoulder pain and improve function. However, results reportedly deteriorate as patients approach mid-term follow-up and little is known about how this impacts physical health-related quality of life (PHRQOL) and mental health-related quality of life (MHRQOL). The study hypothesis was that shoulder function, pain, and medication use for pain would influence PHRQOL and MHRQOL.
Methods
This prospective cohort study involving subjects from 6 orthopedic clinics and 12 fellowship-trained surgeons evaluated the influence of RTSA on PHRQOL, MHRQOL, shoulder function, pain, instability, and medication use over the initial 7 years of a 10-year study, and device survivorship and revision rates. Clinical examination, the American Shoulder and Elbow Surgeons (ASES) score, Short Form (SF)-12 PHRQOL and MHRQOL assessments, the single assessment numeric shoulder function evaluation (SANE), visual analog scale (VAS) shoulder pain and instability scores, shoulder pain, medication use for pain, surgery satisfaction, survivorship and revision rate data were collected pre-RTSA, and at 6-week, 6-month, 1-year, 2-year, 3-year, 5-year, and 7-year follow-ups.
Results
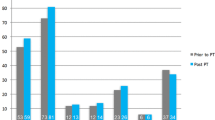
Two hundred participants (108 female) of 69 ± 8.3 years of age, with gross rotator cuff deficiency (poor tissue quality or impaired dynamic stability) (n = 92), glenohumeral joint osteoarthritis (n = 88), failed primary total shoulder arthroplasty (n = 8), non-united humeral head fracture (n = 6) or 3–4 section comminuted humeral head fracture (n = 6) underwent pre-RTSA evaluation. Device survivorship was 94%. Friedman two-way ANOVA and Wilcoxon test pairwise comparisons revealed that compared to pre-RTSA, median active shoulder flexion (+ 25°) and external rotation (+ 10°) mobility improved by 6 months (p < 0.0001) and remained improved. Shoulder flexion (+ 1 grade), abduction, external rotation (+ 0.5 grade), and internal rotation strength (+ 1 grade) also improved by 6 months (p < 0.0001) and remained improved. ASES (+ 26.8), SANE (+ 17.5) and VAS pain (− 5.7) scores improved by 6 weeks (p < 0.0001) and remained improved, as medication use for shoulder pain decreased (− 24.6%) (p < 0.0001). SF-12 PHRQOL scores improved by 6 months (+ 11.5) and remained improved (p < 0.0001). Significant Spearman Rho correlations were observed between shoulder function (ASES or SANE) and SF-12 PHRQOL (r ≥ 0.52) and MHRQOL (r ≥ 0.20) scores (p < 0.0001) supporting the relationship between shoulder function and quality of life. Trend analysis revealed changing shoulder function, pain, and PHRQOL relationships between 2 and 3 years, and 5 and 7 years post-RTSA (Chi-Square, p < 0.05).
Conclusion
Excellent device survival and good-to-excellent perceived shoulder function, and PHRQOL improvements were observed. Secondary objectives of improved shoulder mobility, strength, pain and instability were also achieved. In contrast to previous reports, subjects did not display shoulder mobility or perceived function deterioration by the 7-year follow-up. Following chronic pain relief at 6 weeks post-RTSA, subjects appear to balance PHRQOL and shoulder pain relationships at the 6-month and 1-year post-RTSA follow-ups. Careful evaluation at this time may help patients with higher pain levels and lower function expectations reverse these trends, or patients with lower pain levels and higher function expectations to optimize RTSA use and longevity.





Similar content being viewed by others
Data availability
The data that support study findings are available upon reasonable request from the corresponding author [JN]. The data are not publicly available due to ongoing research study restrictions as some information might compromise participant privacy.
References
Tangtiphailboontana J, Mara KC, Jensen AR, Camp CL, Morrey ME, Sanchez-Sotelo J (2021) Return to sports after primary reverse shoulder arthroplasty. Outcomes at mean 4-year follow-up. Orthop J Sports Med 9(6):23259671211012393. https://doi.org/10.1177/23259671211012393
Guery J, Favard L, Sirveax F, Oudet D, Mole D, Walch G (2006) Reverse total shoulder arthroplasty. J Bone Jt Surg Am 88(8):1742–1747. https://doi.org/10.2106/JBJS.E.00851
Castricini R, Gasparini G, Di Luggo F, De Benedetto M, De Gori M, Galasso O (2013) Health-related quality of life and functionality after reverse shoulder arthroplasty. J Shoulder Elbow Surg 22:1639–1649. https://doi.org/10.1016/j.jse.2013.01.020
Rauck RC, Ruzbarsky JJ, Swarup I, Gruskay J, Dines JS, Warren RF, Dines DM, Gulotta LV (2020) Predictors of patient satisfaction after reverse shoulder arthroplasty. J Shoulder Elbow Surg 29:e67–e74. https://doi.org/10.1016/j.jse.2019.07.043
Christensen J, Brockmeier S (2018) Total shoulder arthroplasty in the athlete and active individual. Clin Sports Med 37:549–558. https://doi.org/10.1016/j.csm.2018.05.005
Wang J, Popchak A, Giugale J, Irrgang J, Lin A (2018) Sports participation is an appropriate expectation for recreational athletes undergoing shoulder arthroplasty. Orthop J Sports Med 6(10):2325967118800666. https://doi.org/10.1177/2325967118800666
Garcia GH, Taylor SA, DePalma BJ, Mahony GT, Grawe BM, Nguyen J, Dines JS, Dines DM, Warren RF, Craig EV, Gulotta VL (2015) Patient activity levels after reverse total shoulder arthroplasty. Am J Sports Med 23(11):2816–2821. https://doi.org/10.1177/0363546515597673
Best MJ, Aziz KT, Wilckens JH, McFarland EG, Srikumaran U (2021) Increasing incidence of primary reverse and anatomic total shoulder arthroplasty in the United States. J Shoulder Elbow Surg 30:1159–1166
Havens E, Slabaugh SL, Helmick CG et al (2017) Comorbid arthritis is associated with lower health-related quality of life in older adults with other chronic conditions, United States, 2013–2014. Prev Chronic Dis 14:E60. https://doi.org/10.5888/pcd14.160495
Jia H, Lubetkin EI, DeMichele K, Stark DS, Zack MM, Thompson WW (2019) Quality-adjusted life years (QALYs) associated with limitations in activities of daily living (ADL) in a large longitudinal sample of the US community-dwelling older population. Disabil Health J 12(4):699–705. https://doi.org/10.1016/j.dhjo.2019.05.003
Jia H, Lubetkin EI, Barile JP et al (2018) Quality-adjusted life years (QALY) for 15 chronic conditions and combinations of conditions among US adults aged 65 and older. Med Care 56(8):740–746. https://doi.org/10.1097/MLR.0000000000000943
Gowd AK, Charles MD, Liu JN, Lalehzarian SP, Cabarcas BC, Manderle BJ, Nicholson GP, Romeo AA, Verma NN (2019) Single assessment numeric evaluation (SANE) is a reliable metric to measure clinically significant improvements following shoulder arthroplasty. J Shoulder Elbow Surg 28:2238–2246. https://doi.org/10.1016/j.jse.2019.04.041
Bachman D, Nyland J, Krupp R (2016) Reverse-total shoulder arthroplasty cost-effectiveness: a quality-adjusted life years comparison with total hip arthroplasty. World J Orthop 7(2):123–127. https://doi.org/10.5312/wjo.v7.i2.123
Shigley C, Green A (2021) Shoulder conditions and health related quality of life and utility: a current concepts review. JSES Int 6(1):167–174
Frankle M, Siegal S, Pupello D, Saleem A, Mighell VM (2005) The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency: A minimum two-year, follow-up of sixty patients. J Bone Jt Surg Am 87:1697–1705
Boudreau S, Boudreau E, Higgins LD, Wilcox RB III (2007) Rehabilitation following reverse total shoulder arthroplasty. J Orthop Sports Phys Ther 37(12):734–746. https://doi.org/10.2519/jospt.2007.2562
Richards RR, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, Iannotti JP, Mow VC, Sidles JA, Zuckerman JD (1994) A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg 3(6):347–352. https://doi.org/10.1016/S1058-2746(09)80019-0
Kendall FP, Kendall FP (2005) Muscles: Testing and function with posture and pain. Lippincott Williams & Wilkins, Baltimore (ISBN: 0-7817-4780-5)
Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC (1999) Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med 27:214–221. https://doi.org/10.1177/03635465990270021701
Ware J Jr, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233. https://doi.org/10.1097/00005650-199603000-00003
Resnick B, Nahm ES (2001) Reliability and validity testing of the revised 12-item Short-Form Health Survey in older adults. J Nurs Meas 9(2):151–161 (PMID: 11696939)
Ware J, Kosinski M, Keller S (1995) SF-12: how to score the SF-12 physical and mental summary scales, 2nd edn. The Health Institute, New England Medical Center, Boston (ISBN: 1891810022 9781891810022)
Chamberlain AM, Hung M, Chen W, Keener JA, McAllister J, Ebersole G, Granger EK, Bowen RC, Tashjian RZ (2017) Determining the patient acceptable symptomatic state for the ASES, SST, and VAS pain after total shoulder arthroplasty. J Shoulder Elbow Arthroplasty 1:1–6. https://doi.org/10.1177/2471549217720042
Su F, Allahabadi S, Bongbong DN, Feeley BT, Landsdown DA (2021) Minimal clinically important difference, substantial clinical benefit, and patient acceptable symptom state of outcome measurements relating to shoulder pathology and surgery: a systematic review. Curr Rev Musculoskel Med 14:27–46. https://doi.org/10.1007/s12178-020-09684-2
Cole EW, Moulton SG, Werner BC, Denard PJ (2022) Why patients fail to achieve a Patient Acceptable Symptom State (PASS) after total shoulder arthroplasty? JSES Int 6:49–55. https://doi.org/10.1016/j.jseint.2021.09.017
Wong SE, Zhang AL, Berliner JL, Ma CB, Feeley BT (2016) Preoperative patient-reported scores can predict postoperative outcomes after shoulder arthroplasty. J Shoulder Elbow Surg 25:913–919. https://doi.org/10.1016/j.jse.2016.01.029
Mukaka MM (2012) Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J 24(3):69–71 (PMID: 23638278)
Portney LG, Watkins MP (1999) Foundations of clinical research: applications to practice, 2nd. Pearson/Prentice Hall, Upper Saddle River (ISBN-13: 978-0838526958)
Risner B, Nyland J, Crawford CH 3rd, Roberts CS, Johnson JR (2008) Orthopaedic in-training examination performance: a nine-year review of a residency program database. South Med J 101(8):791–796
Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff: Results of a multicenter study of 80 shoulders. J Bone Jt Surg Br 86:388–395
Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G (2006) Reverse total shoulder arthroplasty. J Bone Jt Surg Am 88(8):1742–1747
Favard L, Levigne C, Nerot C, Gerber C, De Wilde L, Mole D (2011) Reverse prostheses in arthropathies with cuff tear: are survivorship and function maintained over time? Clin Orthop Relat Res 469:2469–2475
Bacle G, Nove-Josserand L, Garaud P, Walch G (2017) Long-term outcomes of reverse total shoulder arthroplasty: a follow-up of a previous study. J Bone Joint Surg Am 99:454–461
Cuff DJ, Pupello DR, Santoni BG, Clark RE, Frankle MA (2017) Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency. J Bone Joint Surg Am 99:1895–1899
McFarland EG, Meshram P, Rojas J, Joseph J, Srikumaran U (2021) Reverse total shoulder arthroplasty without bone-grafting for severe glenoid bone loss in patients with osteoarthritis and intact rotator cuff: A concise 5-year follow-up of a previous report. J Bone Joint Surg Am 103:581–585
Nyland J, Kanouse Z, Krupp R, Caborn D, Jakob R (2011) Total knee arthroplasty in motivated patients with knee osteoarthritis and athletic activity approach type goals: a conceptual decision-making model. Disabil Rehabil 33:17–18. https://doi.org/10.3109/09638288.2010.533816
Raffaeli W, Arnaudo E (2017) Pain as a disease: an overview. J Pain Res 10:2003–2008. https://doi.org/10.2147/JPR.S138864
Halli-Tierney AD, Scarbrough C, Carroll D (2019) Polypharmacy: evaluating risks and deprescribing. Am Fam Physician 100(1):32–38 (PMID: 31259501)
Sallis RE (2009) Exercise is medicine and physicians need to prescribe it! Br J Sports Med 43:3–4. https://doi.org/10.1136/bjsm.2008.054825
Zimmermann GR, Lehár J, Keith CT (2007) Multi-target therapeutics: when the whole is greater than the sum of the parts. Drug Discov Today 12(1–2):34–42. https://doi.org/10.1016/j.drudis.2006.11.008
Acknowledgements
Thanks to Drs. Brian Feeley, Matthew Ramsey, Luke Austin, Bradford Tucker, Matthew Pepe, and Surena Namdari for referring patients for study participation.
Funding
This study was funded by Zimmer-Biomet.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Ryan Krupp receives consulting fees from Zimmer Biomet and Stryker, and honoraria from Zimmer Biomet, Stryker, and Arthrex; Dr. C. Benjamin Ma receives research funding from Aesculap, the National Institutes of Health, Zimmer Biomet and Stryker, consulting fees from Stryker and ConMed, and royalties from ConMed and SLACK; Dr. John Nyland has no disclosures; Dr. Charles L. Getz receives royalties from Zimmer Biomet, and consulting fees from Depuy Mitek; Dr. Makaram Srinivasan serves as a consultant for Zimmer Biomet.
Ethical approval
This study with human subjects was approved by the medical institutional review boards.
Informed consent
All the study subjects provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Krupp, R., Ma, C.B., Nyland, J. et al. Reverse total shoulder arthroplasty pain and function: new perspectives from a 10-year multicenter study at the 7-year follow-up. Arch Orthop Trauma Surg 143, 4049–4063 (2023). https://doi.org/10.1007/s00402-022-04702-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04702-z