Abstract
Introduction
Excessive version and inclination of the glenoid component during total shoulder arthroplasty can lead to glenohumeral instability, early loosening, and even failure. The orientation and position of the central pin determine the version and inclination of the glenoid component. The purpose of this study was to compare the differences in centerline position and orientation obtained using "3D preoperative planning based on the best-fit method for glenoid elements" and the surgeon's manipulation.
Materials and methods
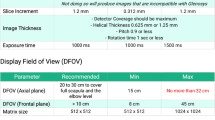
Twenty-nine CT images of glenohumeral osteoarthritis of the shoulder were reconstructed into a 3D model, and a 3D printer was used to create an in vitro model for the surgeon to drill the center pin. The 3D shoulder model was also used for 3D preoperative planning (3DPP) using the best-fit method for glenoid elements. The in vitro model was scanned and the version, inclination and center position were measured to compare with the 3DPP results.
Results
The respective mean inclinations (versions) of the surgeon and 3DPP were −2.63° ± 6.60 (2.87° ± 5.97) and −1.96° ± 4.24 (−3.21° ± 4.00), respectively. There was no significant difference in the inclination and version of the surgeon and 3DPP. For surgeons, the probability of the inclination and version being greater than 10° was 13.8% (4/29) and 10.3% (3/29), respectively. Compared to the 3DPP results, the surgeon's center position was shifted down an average of 1.63 mm. There was a significant difference in the center position of the surgeon and 3DPP (p < 0.05).
Conclusion
The central pin drilled by surgeons using general instruments was significantly lower than those defined using 3D preoperative planning and standard central definitions. 3D preoperative planning prevents the version and inclination of the centerline from exceeding safe values (± 10°).









Similar content being viewed by others
Data availability
The data that support the findings of this study are openly available in [Seminars in Arthroplasty] at https://doi.org/10.1053/j.sart.2017.05.005, reference number [Volume 28, Issue 1, March 2017, Pages 25–29].
Abbreviations
- 3DPP:
-
3D preoperative planning
- PSI:
-
Patient-specific instrumentation
- CAD:
-
Computer-aided design
- MCL:
-
Manual centerline
- SCL:
-
Standard centerline
- ACL:
-
Alternate centerline
- BCL:
-
The centerline of the best-fit implant
- ABS:
-
Acrylonitrile butadiene styrene
- ICP:
-
Iterative closest point algorithm
- GC:
-
The center of the glenoid surface
- E CP_dis :
-
The distance between the center position and the GC
- Max. + Y :
-
The maximum center positions of each centerline in the superior direction
- Max. −Y :
-
The maximum center positions of each centerline in the inferior direction
- Max. + Z :
-
The maximum center positions of each centerline in the anterior direction
- Max.−Z :
-
The maximum center positions of each centerline in the posterior direction
References
Berhouet J, Gulotta L, Dines D, Craig E, Warren R, Choi D et al (2017) Preoperative planning for accurate glenoid component positioning in reverse shoulder arthroplasty. Orthop Traumatol Surg Res 103(3):407–413. https://doi.org/10.1016/j.otsr.2016.12.019
Berhouet J, Jacquot A, Walch G, Deransart P, Favard L, Gauci M et al (2021) Pre-operative planning of baseplate position in reverse shoulder arthroplasty: still no consensus on lateralization, version and inclination. Orthop Traumatol Surg Res 108:103115. https://doi.org/10.1016/j.otsr.2021.103115
Besl PJ, McKay ND (1992) Method for registration of 3-D shapes. IEEE Trans Pattern Anal Mach Intell 14(2):239–256. https://doi.org/10.1117/12.57955
Boileau P, Cheval D, Gauci M-O, Holzer N, Chaoui J, Walch G (2018) Automated three-dimensional measurement of glenoid version and inclination in arthritic shoulders. JBJS 100(1):57–65. https://doi.org/10.2106/jbjs.16.01122
Bolles RC, Fischler MA (1981) RANSAC-based approach to model fitting and its application to finding cylinders in range data. IJCAI 637–643
Burns DM, Frank T, Whyne CM, Henry PDG (2019) Glenoid component positioning and guidance techniques in anatomic and reverse total shoulder arthroplasty: a systematic review and meta-analysis. Shoulder Elbow 11(2_suppl):16–28. https://doi.org/10.1177/1758573218806252
Cabarcas BC, Cvetanovich GL, Gowd AK, Liu JN, Manderle BJ, Verma NN (2019) Accuracy of patient-specific instrumentation in shoulder arthroplasty: a systematic review and meta-analysis. JSES Open Access 3(3):117–129. https://doi.org/10.1016/j.jses.2019.07.002
Chae J, Siljander M, Wiater JM (2018) Instability in reverse total shoulder arthroplasty. JAAOS 26(17):587–596. https://doi.org/10.5435/JAAOS-D-16-00408
Dallalana RJ, McMahon RA, East B, Geraghty L (2016) Accuracy of patient-specific instrumentation in anatomic and reverse total shoulder arthroplasty. Int J Shoulder Surg 10(2):59. https://doi.org/10.4103/0973-6042.180717
Denard PJ, Provencher MT, Lädermann A, Romeo AA, Parsons BO, Dines JS (2018) Version and inclination obtained with 3-dimensional planning in total shoulder arthroplasty: do different programs produce the same results? JSES Open Access 2(4):200–204. https://doi.org/10.1016/j.jses.2018.06.003
Erickson BJ, Chalmers PN, Denard P, Lederman E, Horneff G, Werner BC et al (2021) Does commercially available shoulder arthroplasty preoperative planning software agree with surgeon measurements of version, inclination, and subluxation? J Shoulder Elbow Surg 30(2):413–420. https://doi.org/10.1016/j.jse.2020.05.027
Familiari F, Huri G, McFarland EG (2014) Supraspinatus tears after total shoulder arthroplasty: a review of diagnosis and treatment. Semin Arthroplasty 25(1):64–70. https://doi.org/10.1053/j.sart.2014.02.011
Frankle MA, Teramoto A, Luo Z-P, Levy JC, Pupello D (2009) Glenoid morphology in reverse shoulder arthroplasty: classification and surgical implications. J Shoulder Elbow Surg 18(6):874–885. https://doi.org/10.1016/j.jse.2009.02.013
Goetti P, Denard PJ, Collin P, Ibrahim M, Mazzolari A, Lädermann A (2021) Biomechanics of anatomic and reverse shoulder arthroplasty. EFORT Open Rev 6(10):918–931. https://doi.org/10.1302/2058-5241.6.210014
Gregory TM, Sankey A, Augereau B, Vandenbussche E, Amis A, Emery R et al (2013) Accuracy of glenoid component placement in total shoulder arthroplasty and its effect on clinical and radiological outcome in a retrospective, longitudinal, monocentric open study. PLoS ONE 8(10):e75791. https://doi.org/10.1371/journal.pone.0075791
Iannotti JP, Davidson IU, Ricchetti ET (2017) Three-dimensional preoperative planning and patient-specific instrumentation for total shoulder arthroplasty. Semin Arthroplasty 28(1):25–29. https://doi.org/10.1053/j.sart.2017.05.005
Iannotti JP, Walker K, Rodriguez E, Patterson TE, Jun BJ, Ricchetti ET (2019) Accuracy of 3-dimensional planning, implant templating, and patient-specific instrumentation in anatomic total shoulder arthroplasty. JBJS 101(5):446–457. https://doi.org/10.2106/JBJS.17.01614
Jacquot A, Gauci M-O, Chaoui J, Baba M, Deransart P, Boileau P et al (2018) Proper benefit of a three dimensional pre-operative planning software for glenoid component positioning in total shoulder arthroplasty. Int Orthop 42(12):2897–2906. https://doi.org/10.1007/s00264-018-4037-1
Keener JD, Patterson BM, Orvets N, Aleem AW, Chamberlain AM (2018) Optimizing reverse shoulder arthroplasty component position in the setting of advanced arthritis with posterior glenoid erosion: a computer-enhanced range of motion analysis. J Shoulder Elbow Surg 27(2):339–349. https://doi.org/10.1016/j.jse.2017.09.011
Levins JG, Kukreja M, Paxton ES, Green AJ (2021) Computer-assisted preoperative planning and patient-specific instrumentation for glenoid implants in shoulder arthroplasty. JBJS Rev 9(9):e20. https://doi.org/10.2106/JBJS.RVW.20.00236
Levy JC, Everding NG, Frankle MA, Keppler LJ (2014) Accuracy of patient-specific guided glenoid component positioning for reverse shoulder arthroplasty. J Shoulder Elbow Surg 23(10):1563–1567. https://doi.org/10.1016/j.jse.2014.01.051
Lewis GS, Armstrong AD (2011) Glenoid spherical orientation and version. J Shoulder Elbow Surg 20(1):3–11. https://doi.org/10.1016/j.jse.2010.05.012
Netto N (2021) The role of 3D printing in the positioning of the glenoidal component in total shoulder arthroplasty. Clin Surg 6(13):1–6
Ozel O, Hudek R, Abdrabou MS, Werner BS, Gohlke F (2020) The implications of the glenoid angles and rotator cuff status in patients with osteoarthritis undergoing shoulder arthroplasty. BMC Musculoskelet Disord 21(1):1–8. https://doi.org/10.1186/s12891-020-03690-8
Raiss P, Walch G, Wittmann T, Athwal GS (2020) Is preoperative planning effective for intraoperative glenoid implant size and type selection during anatomic and reverse shoulder arthroplasty? J Shoulder Elbow Surg 29(10):2123–2127. https://doi.org/10.1016/j.jse.2020.01.098
Reid JJ, Kunkle BF, Greene AT, Eichinger JK, Friedman RJ (2021) Variability and reliability of 2-dimensional vs. 3-dimensional glenoid version measurements with 3-dimensional preoperative planning software. J Shoulder Elbow Surg 31(2):302–309. https://doi.org/10.1016/j.jse.2021.07.011
Ricchetti ET, Jun B-J, Jin Y, Entezari V, Patterson TE, Derwin KA et al (2021) Three-dimensional computed tomography analysis of pathologic correction in total shoulder arthroplasty based on severity of preoperative pathology. J Shoulder Elbow Surg 30(2):237–249. https://doi.org/10.1016/j.jse.2020.07.033
Rosenthal Y, Rettig SA, Virk MS, Zuckerman JD (2020) Impact of preoperative 3-dimensional planning and intraoperative navigation of shoulder arthroplasty on implant selection and operative time: a single surgeon’s experience. J Shoulder Elbow Surg 29(12):2564–2570. https://doi.org/10.1016/j.jse.2020.03.041
Sabesan VJ, Ackerman J, Sharma V, Baker KC, Kurdziel MD, Wiater JM et al (2015) Glenohumeral mismatch affects micromotion of cemented glenoid components in total shoulder arthroplasty. J Shoulder Elbow Surg 24(5):814–822. https://doi.org/10.1016/j.jse.2014.10.004
Sabesan VJ, Lima DJ, Rudraraju RT, Wilneff M, Sheth B, Yawman J (2020) Reliability and accuracy of 3D preoperative planning software for glenoid implants in total shoulder arthroplasty. Semin Arthroplasty 30(4):375–382. https://doi.org/10.1053/j.sart.2020.09.010
Sabesan VJ, Rudraraju RT, Sheth B, Grauer J, Stankard M, Chatha K et al (2020) Three-dimensional preoperative planning accurately guides surgeons for intraoperative implant selection in shoulder arthroplasty. Semin Arthroplasty 30(4):360–367. https://doi.org/10.1053/j.sart.2020.08.009
Schoch BS, Haupt E, Leonor T, Farmer KW, Wright TW, King J et al (2020) Computer navigation leads to more accurate glenoid targeting during total shoulder arthroplasty compared with 3-dimensional preoperative planning alone. J Shoulder Elbow Surg 29(11):2257–2263. https://doi.org/10.1016/j.jse.2020.03.014
Shah SS, Sahota S, Denard PJ, Provencher MT, Parsons BO, Hartzler RU et al (2019) Variability in total shoulder arthroplasty planning software compared to a control CT-derived 3D printed scapula. Shoulder Elbow 13(3):268–275. https://doi.org/10.1177/1758573219888821
Terrier A, Ston J, Larrea X, Farron A (2014) Measurements of three-dimensional glenoid erosion when planning the prosthetic replacement of osteoarthritic shoulders. Bone Jt J 96(4):513–518. https://doi.org/10.1302/0301-620X.96B4.32641
Theopold J, Pieroh P, Scharge M, Marquaß B, Hohmann T, Josten C et al (2016) Improved accuracy of K-wire positioning into the glenoid vault by intraoperative 3D image intensifier-based navigation for the glenoid component in shoulder arthroplasty. Orthop Traumatol Surg Res 102(5):575–581. https://doi.org/10.1016/j.otsr.2016.03.013
Throckmorton TW, Gulotta LV, Bonnarens FO, Wright SA, Hartzell JL, Rozzi WB et al (2015) Patient-specific targeting guides compared with traditional instrumentation for glenoid component placement in shoulder arthroplasty: a multi-surgeon study in 70 arthritic cadaver specimens. J Shoulder Elbow Surg 24(6):965–971. https://doi.org/10.1016/j.jse.2014.10.013
Verborgt O, Hachem A, Eid K, Vuylsteke K, Ferrand M, Hardy P et al (2018) Accuracy of patient-specific guided implantation of the glenoid component in reversed shoulder arthroplasty. Orthop Traumatol Surg Res 104(6):767–772. https://doi.org/10.1016/j.otsr.2018.01.010
Villatte G, Muller A-S, Pereira B, Mulliez A, Reilly P, Emery R (2018) Use of patient-specific instrumentation (PSI) for glenoid component positioning in shoulder arthroplasty. A systematic review and meta-analysis. PloS one 13(8):e0201759. https://doi.org/10.1371/journal.pone.0201759
Werner BS, Hudek R, Burkhart KJ, Gohlke F (2017) The influence of three-dimensional planning on decision-making in total shoulder arthroplasty. J Shoulder Elbow Surg 26(8):1477–1483. https://doi.org/10.1016/j.jse.2017.01.006
Yam MGJ, Chao JYY, Leong C, Tan CH (2021) 3D printed patient specific customised surgical jig for reverse shoulder arthroplasty, a cost effective and accurate solution. J Clin Orthop Trauma 21:101503. https://doi.org/10.1016/j.jcot.2021.101503
Yongpravat C, Lester JD, Saifi C, Trubelja A, Greiwe RM, Bigliani LU et al (2013) Glenoid morphology after reaming in computer-simulated total shoulder arthroplasty. J Shoulder Elbow Surg 22(1):122–128. https://doi.org/10.1016/j.jse.2011.12.010
Acknowledgements
The authors thank Chang Gung Memorial Hospital (GMRPG3H1741) for funding this study and Horng Bang International Co., Ltd, Taiwan, providing 3D scanning device and technology.
Funding
This project was supported by cooperative research from Chang Gung Memorial Hospital (GMRPG3H1741). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the donor.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors Chi-Pin Hsu, Chen-Te Wu, Chao-Yu Chen, Shang-Chih Lin,and Kuo-Yao Hsu, their immediate families and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity that are related to the subject of this article.
Ethics approval
This study was granted an exemption by the Chang Gung Memorial Hospital Institutional Review Board (Protocol No. 201701867B0C501).
Informed consent
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hsu, CP., Wu, CT., Chen, CY. et al. Difference analysis of the glenoid centerline between 3D preoperative planning and 3D printed prosthesis manipulation in total shoulder arthroplasty. Arch Orthop Trauma Surg 143, 4065–4075 (2023). https://doi.org/10.1007/s00402-022-04688-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04688-8