Abstract
Purpose
Treatment of chronic lateral ankle instability (CLAI) with poor remnant quality is challenging. The aim of the present study was to evaluate clinical results and complications of anatomic reconstruction of the lateral ligaments using allograft tendon and suspensory fixation in the treatment of such patients.
Methods
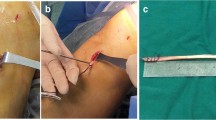
One hundred and eight patients with CLAI, who were treated surgically using anatomic reconstruction with allograft tendon and suspensory fixation between April 2016 and January 2018 at our hospital, were retrospectively analysed. None of the patients had sufficient ligament remnants for the modified Broström procedure during the intraoperative evaluation. Eighteen patients were excluded. Seventeen patients were lost to follow-up and 73 patients completed the study. The mean duration of instability symptoms was 39.1 months (range, 6–480 months). The mean follow-up time was 57.5 months (range, 48–69 months). Clinical results were evaluated using the Karlsson scoring scale, American Orthopaedic Foot and Ankle Society-Ankle and Hindfoot (AOFAS-AH) score, visual analogue scale (VAS), patients’ subjective satisfaction, and incidence of complications. Mechanical stability was evaluated using the varus talar tilt angle (TTA) and anterior talar displacement (ATD).
Results
The AOFAS-AH scores significantly improved from 67.7 ± 8.5 points to 89.8 ± 9.5 (p < 0.001). The Karlsson scoring scales evolved from 58.8 ± 16.5 to 88.4 ± 11.2 (p < 0.001). VAS scores significantly decreased from 2.9 ± 1.3 to 1.1 ± 1.0 (p < 0.001). On stress radiographs, TTA decreased from 15.1 ± 2.5 degrees to 5.8 ± 2.1 degrees (p < 0.001), whereas ATD reduced from 13.4 ± 2.9 mm to 5.7 ± 1.5 mm (p < 0.001). Patients' subjective satisfaction indicated 46 excellent, 20 good, 5 fair, and 2 bad results. Postoperatively, 15 cases (20.5%) did not achieve complete relief of discomfort or swelling, 9 cases (12.3%) experienced joint stiffness or decreased range of motion, and 6 cases (8.2%) had soft tissue irritation. Residual instability and reoperation are rare. Allograft rejection or wound infection was not observed.
Conclusion
For the CLAI patients with poor remnant quality, anatomic reconstruction of the lateral ligaments using allograft tendon and suspensory fixation is an effective procedure, while the top three complications in incidence were residual discomfort, joint stiffness, and soft tissue irritation.
Levels of evidence
Level IV, retrospective case series.

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Change history
24 November 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00402-022-04699-5
References
Bell SJ, Mologne TS, Sitler DF, Cox JS (2006) Twenty-six-year results after Brostrom procedure for chronic lateral ankle instability. Am J Sports Med 34:975–978
Boniello MR, Schwingler PM, Bonner JM, Robinson SP, Cotter A, Bonner KF (2015) Impact of hamstring graft diameter on tendon strength: a biomechanical study. Arthroscopy 31:1084–1090
Boutsiadis A, Brossard P, Panisset JC, Graveleau N, Barth J (2017) Minimally invasive combined anterior and anterolateral stabilization of the knee using hamstring tendons and adjustable-loop suspensory fixation device: surgical technique. Arthrosc Tech 6:e419–e425
Cao Y, Xu Y, Hong Y, Xu X (2018) A new minimally invasive method for anatomic reconstruction of the lateral ankle ligaments with a Tightrope system. Arch Orthop Trauma Surg 138:1549–1555
Dierckman BD, Ferkel RD (2015) Anatomic reconstruction with a semitendinosus allograft for chronic lateral ankle instability. Am J Sports Med 43:1941–1950
Eble SK, Hansen OB, Patel KA, Drakos MC (2021) Lateral ligament reconstruction with hamstring graft for ankle instability: outcomes for primary and revision cases. Am J Sports Med 49:2697–2706
Guillo S, Bauer T, Lee JW, Takao M, Kong SW, Stone JW et al (2013) Consensus in chronic ankle instability: aetiology, assessment, surgical indications and place for arthroscopy. Orthop Traumatol Surg Res 99:S411-419
Halabchi F, Angoorani H, Mirshahi M, Pourgharib Shahi MH, Mansournia MA (2016) The prevalence of selected intrinsic risk factors for ankle sprain among elite football and basketball players. Asian J Sports Med 7:e35287
Hayback G, Raas C, Rosenberger R (2021) Failure rates of common grafts used in ACL reconstructions: a systematic review of studies published in the last decade. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04147-w
Hershkovich O, Tenenbaum S, Gordon B, Bruck N, Thein R, Derazne E et al (2015) A large-scale study on epidemiology and risk factors for chronic ankle instability in young adults. J Foot Ankle Surg 54:183–187
Hollis JM, Blasier RD, Flahiff CM, Hofmann OE (1995) Biomechanical comparison of reconstruction techniques in simulated lateral ankle ligament injury. Am J Sports Med 23:678–682
Kim HN, Dong Q, Hong do Y, Yoon YH, Park YW (2014) Percutaneous lateral ankle ligament reconstruction using a split peroneus longus tendon free graft: technical tip. Foot Ankle Int 35:1082–1086
Krips R, Brandsson S, Swensson C, van Dijk CN, Karlsson J (2002) Anatomical reconstruction and Evans tenodesis of the lateral ligaments of the ankle. Clinical and radiological findings after follow-up for 15 to 30 years. J Bone Joint Surg Br 84:232–236
Krych AJ, Jackson JD, Hoskin TL, Dahm DL (2008) A meta-analysis of patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction. Arthroscopy 24:292–298
Lan R, Piatt ET, Bolia IK, Haratian A, Hasan L, Peterson AB et al (2021) Suture tape augmentation in lateral ankle ligament surgery: current concepts review. Foot Ankle Orthop 6:24730114211045976
Lan S, Zeng W, Yuan G, Xu F, Cai X, Tang M et al (2020) All-inside arthroscopic anterior talofibular ligament anatomic reconstruction with a gracilis tendon autograft for chronic ankle instability in high-demand patients. J Foot Ankle Surg 59:222–230
Mederake M, Hofmann UK, Ipach I (2021) Arthroscopic modified Brostrom operation versus open reconstruction with local periosteal flap in chronic ankle instability. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-03949-2
Neuschwander TB, Indresano AA, Hughes TH, Smith BW (2013) Footprint of the lateral ligament complex of the ankle. Foot Ankle Int 34:582–586
Park KH, Lee JW, Suh JW, Shin MH, Choi WJ (2016) Generalized ligamentous laxity is an independent predictor of poor outcomes after the modified brostrom procedure for chronic lateral ankle instability. Am J Sports Med 44:2975–2983
Petrera M, Dwyer T, Theodoropoulos JS, Ogilvie-Harris DJ (2014) Short- to medium-term outcomes after a modified brostrom repair for lateral ankle instability with immediate postoperative weightbearing. Am J Sports Med 42:1542–1548
Rupp MC, Degenhardt H, Winkler PW, Hinz M, Ehmann YJ, Imhoff AB et al (2022) High return to sports and return to work rates after anatomic lateral ankle ligament reconstruction with tendon autograft for isolated chronic lateral ankle instability. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-06937-0
Samejima Y, Inokuchi R, Iwashita K, Ikegami H, Musha Y, Jujo Y et al (2021) Arthroscopic ankle lateral ligament repair alone versus arthroscopic ankle lateral ligament repair with reinforcement by inferior extensor retinaculum. Arch Orthop Trauma Surg 141:987–995
Shibuya N, Bazan DI, Evans AM, Agarwal MR, Jupiter DC (2016) Efficacy and safety of split peroneal tendon lateral ankle stabilization. J Foot Ankle Surg 55:812–816
St Pierre RK, Rosen J, Whitesides TE, Szczukowski M, Fleming LL, Hutton WC (1983) The tensile strength of the anterior talofibular ligament. Foot Ankle 4:83–85
Strauss JE, Forsberg JA, Lippert FG 3rd (2007) Chronic lateral ankle instability and associated conditions: a rationale for treatment. Foot Ankle Int 28:1041–1044
Su T, Jiang YF, Hou ZC, Zhao YQ, Chen W, Hu YL et al (2022) The L-shaped tunnel technique showed favourable outcomes similar to those of the Y-graft technique in anatomic lateral ankle ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-06880-0
Takao M, Oae K, Uchio Y, Ochi M, Yamamoto H (2005) Anatomical reconstruction of the lateral ligaments of the ankle with a gracilis autograft: a new technique using an interference fit anchoring system. Am J Sports Med 33:814–823
Teixeira J, Guillo S (2018) Arthroscopic treatment of ankle instability - allograft/autograft reconstruction. Foot Ankle Clin 23:571–579
Tian J, Mok TN, Sin TH, Zha Z, Zheng X, Teng Q et al (2021) Clinical outcomes of anterior tibiofibular ligament’s distal fascicle transfer versus ligament reconstruction with InternalBrace for chronic ankle instability patients. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04214-2
van der Wees PJ, Lenssen AF, Hendriks EJM, Stomp DJ, Dekker J, de Bie RA (2006) Effectiveness of exercise therapy and manual mobilisation in acute ankle sprain and functional instability: A systematic review. Australian J Physiotherapy 52:27–37
Vuurberg G, Altink N, Rajai M, Blankevoort L, Kerkhoffs G (2019) Weight, BMI and stability are risk factors associated with lateral ankle sprains and chronic ankle instability: a meta-analysis. J ISAKOS 4:313–327
Wenny R, Duscher D, Meytap E, Weninger P, Hirtler L (2014) Dimensions and attachments of the ankle ligaments: evaluation for ligament reconstruction. Anat Sci Int 90:161–171
Wijnhoud EJ, Rikken QGH, Dahmen J, Sierevelt IN, Stufkens SAS, Kerkhoffs G (2022) One in three patients with chronic lateral ankle instability has a cartilage lesion. Am J Sports Med. https://doi.org/10.1177/03635465221084365
Wittig U, Hohenberger G, Ornig M, Schuh R, Reinbacher P, Leithner A et al (2022) Improved outcome and earlier return to activity after suture tape augmentation versus brostrom repair for chronic lateral ankle instability? A systematic review. Arthroscopy 38:597–608
Funding
This work was supported by the Shanghai Municipal Health Commission (No. 201940339) and the National Natural Science Foundation of China (No. 81772372).
Author information
Authors and Affiliations
Contributions
YC and XX contributed to conception and design. YC, CY, YX, and YH contributed to acquisition of data. CY and YX contributed to analysis and interpretation of data. YC and YH contributed to writing—original draft preparation; XX contributed to writing—review and editing; YC and XX contributed to funding acquisition. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The study was approved by the Ethics Committee of Shanghai Ruijin Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In the “Data availability” section, the final two words “reasonable request” were missing.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cao, Y., Yang, C., Xu, Y. et al. Anatomic reconstruction of the lateral ligaments using allograft tendon and suspensory fixation for chronic lateral ankle instability with poor remnant quality: results and complications. Arch Orthop Trauma Surg 143, 3231–3237 (2023). https://doi.org/10.1007/s00402-022-04680-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04680-2