Abstract
Introduction
Loosening and migration are common modes of aseptic failure following complex revision total knee arthroplasty (rTKA). Metaphyseal cones allow surgeons to negotiate the loss of femoral and tibial bone stock while obtaining stable bony fixation. This study examines the mid-term functional and radiographic outcomes in patients undergoing rTKA utilizing a novel metaphyseal cone system with stems of variable length and fixation methods.
Methods
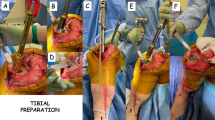
This two-center retrospective study examined all patients who underwent rTKA with a novel porous, titanium tibial or femoral cone in combination with a stem of variable length and fixation who had a minimum follow-up of 2-years. Outcome analysis was separated into tibial and femoral cones as well as the stem fixation method (hybrid vs. fully cemented).
Results
Overall, 123 patients who received 156 cone implants were included (74 [60.2%] tibial only, 16 [13.0%] femoral only, and 33 [26.8%] simultaneous tibial and femoral) with a mean follow-up of 2.76 ± 0.66 years. At 2-years of follow-up the total cohort demonstrated 94.3% freedom from all-cause re-revisions, 97.6% freedom from aseptic re-revisions, and 99.4% of radiographic cone osteointegration. All-cause revision rates did not differ between stem fixation techniques in both the tibial and femoral cone groups.
Conclusion
The use of a novel porous titanium femoral and tibial metaphyseal cones combined with stems in patients with moderate to severe bone defects undergoing complex revision total knee arthroplasty confers excellent results independent of stem fixation technique.
Level of evidence
IV, case series.





Similar content being viewed by others
References
Vasso M, Beaufils P, Cerciello S, Schiavone Panni A (2014) Bone loss following knee arthroplasty: potential treatment options. Arch Orthop Trauma Surg 134:543–553. https://doi.org/10.1007/s00402-014-1941-8
Morgan-Jones R, Oussedik SIS, Graichen H, Haddad FS (2015) Zonal fixation in revision total knee arthroplasty. Bone Joint J 97:147–149. https://doi.org/10.1302/0301-620X.97B2.34144
Ponzio DY, Austin MS (2015) Metaphyseal bone loss in revision knee arthroplasty. Curr Rev Musculoskelet Med 8:361–367. https://doi.org/10.1007/s12178-015-9291-x
Malhotra R, Garg B, Kumar V (2011) Dual massive skeletal allograft in revision total knee arthroplasty. Indian J Orthop. https://doi.org/10.4103/0019-5413.82345
Anderson LA, Christie M, Blackburn BE et al (2021) 3D-printed titanium metaphyseal cones in revision total knee arthroplasty with cemented and cementless stems. Bone Jt J 103:150–157. https://doi.org/10.1302/0301-620X.103B6.BJJ-2020-2504.R1
Behery OA, Shing EZ, Yu Z et al (2021) Survivorship and radiographic evaluation of metaphyseal cones with short cemented stems in revision total knee arthroplasty. J Arthroplasty 37:330–335. https://doi.org/10.1016/j.arth.2021.10.027
Kamath AF, Lewallen DG, Hanssen AD (2015) Porous tantalum metaphyseal cones for severe tibial bone loss in revision knee arthroplasty. J Bone Jt Surg Am 97:216–223. https://doi.org/10.2106/JBJS.N.00540
Tetreault MW, Perry KI, Pagnano MW et al (2020) Excellent two-year survivorship of 3D-printed metaphyseal cones in revision total knee arthroplasty. Bone Jt J 102:107–115. https://doi.org/10.1302/0301-620X.102B6.BJJ-2019-1544.R1
Kang SG, Park CH, Song SJ (2018) Stem fixation in revision total knee arthroplasty: indications, stem dimensions, and fixation methods. Knee Surg Relat Res 30:187–192. https://doi.org/10.5792/ksrr.18.019
Patel AR, Barlow B, Ranawat AS (2015) Stem length in revision total knee arthroplasty. Curr Rev Musculoskelet Med 8:407–412. https://doi.org/10.1007/s12178-015-9297-4
Jacquet C, Ros F, Guy S et al (2021) Trabecular metal cones combined with short cemented stem allow favorable outcomes in aseptic revision total knee arthroplasty. J Arthroplasty 36:657–663. https://doi.org/10.1016/j.arth.2020.08.058
Denehy KM, Abhari S, Krebs VE et al (2019) Metaphyseal fixation using highly porous cones in revision total knee arthroplasty: minimum two year follow up study. J Arthroplasty 34:2439–2443. https://doi.org/10.1016/j.arth.2019.03.045
Engh GA, Ammeen DJ (1999) Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect 48:167–175
Huten D (2013) Femorotibial bone loss during revision total knee arthroplasty. Orthop Traumatol Surg Res 99:S22-33. https://doi.org/10.1016/j.otsr.2012.11.009
Ewald (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 2:2
Fehring TK, Odum S, Olekson C et al (2003) Stem fixation in revision total knee arthroplasty. Clin Orthop Relat Res 416:217–224. https://doi.org/10.1097/01.blo.0000093032.56370.4b
Bottner F, Laskin R, Windsor RE, Haas SB (2006) Hybrid component fixation in revision total knee arthroplasty. Clin Orthop Relat Res 446:127–131. https://doi.org/10.1097/01.blo.0000214418.36959.c5
Wang C, Pfitzner T, von Roth P et al (2016) Fixation of stem in revision of total knee arthroplasty: cemented versus cementless—a meta-analysis. Knee Surg Sport Traumatol Arthrosc 24:3200–3211. https://doi.org/10.1007/s00167-015-3820-4
Lei P, Hu R, Hu Y (2019) Bone defects in revision total knee arthroplasty and management. Orthop Surg 11:15–24. https://doi.org/10.1111/os.12425
Rodríguez-Merchán EC, Gómez-Cardero P, Encinas-Ullán CA (2021) Management of bone loss in revision total knee arthroplasty: therapeutic options and results. EFORT Open Rev 6:1073–1086. https://doi.org/10.1302/2058-5241.6.210007
Erivan R, Tracey R, Mulliez A et al (2021) Medium term clinical outcomes of tibial cones in revision knee arthroplasty. Arch Orthop Trauma Surg 141:113–118. https://doi.org/10.1007/s00402-020-03532-1
Suh C, Se L, Park J, Soo S (2013) The effect of simulated knee flexion on sagittal spinal alignment: novel interpretation of spinopelvic alignment. Eur Spine J. https://doi.org/10.1007/s00586-013-2661-4
Divano S, Cavagnaro L, Zanirato A et al (2018) Porous metal cones: gold standard for massive bone loss in complex revision knee arthroplasty? A systematic review of current literature. Arch Orthop Trauma Surg 138:851–863. https://doi.org/10.1007/s00402-018-2936-7
Chalmers BP, Malfer CM, Mayman DJ et al (2021) Early survivorship of newly designed highly porous metaphyseal tibial cones in revision total knee arthroplasty. Arthroplast Today 8:5–10. https://doi.org/10.1016/j.artd.2021.01.004
Geary MB, Macknet DM, Ransone MP et al (2020) Why do revision total knee arthroplasties fail? A single-center review of 1632 revision total knees comparing historic and modern cohorts. J Arthroplasty 35:2938–2943. https://doi.org/10.1016/j.arth.2020.05.050
Angerame MR, Jennings JM, Holst DC, Dennis DA (2019) Management of bone defects in revision total knee arthroplasty with use of a stepped, porous-coated metaphyseal sleeve. JBJS Essent Surg Tech 9:e14. https://doi.org/10.2106/JBJS.ST.18.00038
Brown NM, Bell JA, Jung EK et al (2015) The use of trabecular metal cones in complex primary and revision total knee arthroplasty. J Arthroplasty 30:90–93. https://doi.org/10.1016/j.arth.2015.02.048
Girerd D, Parratte S, Lunebourg A et al (2016) Total knee arthroplasty revision with trabecular tantalum cones: preliminary retrospective study of 51 patients from two centres with a minimal 2-year follow-up. Orthop Traumatol Surg Res 102:429–433. https://doi.org/10.1016/j.otsr.2016.02.010
Behery OA, Shing EZ, Yu Z et al (2021) Survivorship and radiographic evaluation of metaphyseal cones with short cemented stems in revision total knee arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2021.10.027
Hernandez NM, Hinton ZW, Wu CJ et al (2021) Mid-term results of tibial cones. Bone Joint J 103:158–164. https://doi.org/10.1302/0301-620X.103B6.BJJ-2020-1934.R1
Kosse NM, van Hellemondt GG, Wymenga AB, Heesterbeek PJC (2017) Comparable stability of cemented vs press-fit placed stems in revision total knee arthroplasty with mild to moderate bone loss: 6.5-year results from a randomized controlled trial with radiostereometric analysis. J Arthroplasty 32:197–201. https://doi.org/10.1016/j.arth.2016.06.003
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I.S, C.O, J.W, P.H J.R have nothing to disclose. G.VH reports being a paid consultant for Smith&Nephew. S.M reports being a paid consultant for Zimmer and Intelijoint. R.S reports IP royalties from Smith & Nephew, being paid consultant for Smith & Nephew, Intelijoint, have stock options from Intelijoint, Gauss Surgical and receives research support from Smith & Nephew anddIntelijoint.
Ethical approval
The present study was exempt from human-subjects review by our Institutional Review Board (IRB).
Informed consent
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shichman, I., Oakley, C., Willems, J.H. et al. Novel metaphyseal porous titanium cones allow favorable outcomes in revision total knee arthroplasty. Arch Orthop Trauma Surg 143, 1537–1547 (2023). https://doi.org/10.1007/s00402-022-04645-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04645-5