Abstract
Introduction
To investigate the dynamic aspects of elbow stability, we aimed to analyze sensory nerve endings in the ligaments and the capsule of elbow joints.
Materials and methods
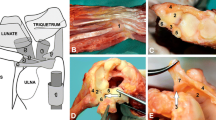
The capsule with its anterior (AJC) and posterior (PJC) parts, the radial collateral ligament (RCL), the annular ligament (AL), and the ulnar collateral ligament with its posterior (PUCL), transverse (TUCL) and anterior parts (AUCL) were dissected from eleven human cadaver elbow joints. Sensory nerve endings were analyzed in two levels per specimen as total cell amount/ cm2 after immunofluorescence staining with low-affinity neurotrophin receptor p75, protein gene product 9.5, S-100 protein and 4′,6-Diamidin-2-phenylindol, Carbonic anhydrase II and choline acetyltransferase on an Apotome microscope according to Freeman and Wyke’s classification.
Results
Free nerve endings were the predominant mechanoreceptor in all seven structures followed by Ruffini, unclassifiable, Golgi-like, and Pacini corpuscles (p ≤ 0.00001, respectively). Free nerve endings were observed significant more often in the AJC than in the RCL (p < 0.00002). A higher density of Ruffini endings than Golgi-like endings was observed in the PJC (p = 0.004). The RCL contained significant more Ruffini endings than Pacini corpuscles (p = 0.004). Carbonic anhydrase II was significantly more frequently positively immunoreactive than choline acetyltransferase in all sensory nerve endings (p < 0.05). Sensory nerve endings were significant more often epifascicular distributed in all structures (p < 0.006, respectively) except for the AJC, which had a pronounced equal distribution (p < 0.00005).
Conclusion
The high density of free nerve endings in the joint capsule indicates that it has pronounced nociceptive functions. Joint position sense is mainly detected by the RCL, AUCL, PUCL, and the PJC. Proprioceptive control of the elbow joint is mainly monitored by the joint capsule and the UCL, respectively. However, the extreme range of motion is primarily controlled by the RCL mediated by Golgi-like endings.












Similar content being viewed by others
References
Soubeyrand M, Assabah B, Bégin M et al (2017) Pronation and supination of the hand: Anatomy and biomechanics. Hand Surg Rehabil 36:2–11. https://doi.org/10.1016/j.hansur.2016.09.012
Juul-Kristensen B, Lund H, Hansen K et al (2008) Poorer elbow proprioception in patients with lateral epicondylitis than in healthy controls: A cross-sectional study. J Shoulder Elb Surg 17:72–81. https://doi.org/10.1016/j.jse.2007.07.003
Siqueira GSL, Amaral MVG, Schiefer M et al (2017) Proprioceptive deficit after total elbow arthroplasty: an observational study. J Shoulder Elb Surg 26:2017–2022. https://doi.org/10.1016/j.jse.2017.07.003
Lubiatowski P, Olczak I, Lisiewicz E et al (2014) Elbow joint position sense after total elbow arthroplasty. J Shoulder Elb Surg 23:693–700. https://doi.org/10.1016/j.jse.2014.01.016
Ettinger LR, Shapiro M, Karduna A (2017) Subacromial anesthetics increase proprioceptive deficit in the shoulder and elbow in patients with subacromial impingement syndrome. Clin Med Insights Arthritis Musculoskelet Disord 10:1–7. https://doi.org/10.1177/1179544117713196
Bryce CD, Armstrong AD (2008) Anatomy and Bbiomechanics of the elbow. Orthop Clin North Am 39:141–154. https://doi.org/10.1016/j.ocl.2007.12.001
Li K, Yi U, Su W, Jen N, Fu H, Wei H, Pickett KA (2015) Kinesthetic deficit in children with developmental coordination disorder. Res Dev Disabil 38:125–133. https://doi.org/10.1016/j.ridd.2014.12.013
Tunik E, Poizner H, Levin MF et al (2003) Arm-trunk coordination in the absence of proprioception. Exp Brain Res 153:343–355. https://doi.org/10.1007/s00221-003-1576-4
Sherrington CS (1906) The integrative action of the nervous system. Archibald Constable & Co. Ltd. London. https://doi.org/10.1017/CBO9781107415324.004
Proske U (2005) What is the role of muscle receptors in proprioception? Muscle Nerve 31:780–787. https://doi.org/10.1002/mus.20330
Crago PE (2019) Neuromodulation by combined sensory and motor stimulation in the peripheral nerve: tendon organ afferent activity. J Neural Eng. https://doi.org/10.1088/1741-2552/aaeaa9
Rein S, Semisch M, Garcia-Elias M et al (2015) Immunohistochemical mapping of sensory nerve endings in the human triangular fibrocartilage complex. Clin Orthop Relat Res 473:3245–3253. https://doi.org/10.1007/s11999-015-4357-z
Rein S, Manthey S, Zwipp H, Witt A (2014) Distribution of sensory nerve endings around the human sinus tarsi: A cadaver study. J Anat 224:499–508. https://doi.org/10.1111/joa.12157
Wyke B (1967) The neurology of joints. Ann R Coll Surg Engl 41:25–50
Cobo R, García-Piqueras J, Cobo J, Vega JA (2021) The human cutaneous sensory corpuscles: An update. J Clin Med 10:227. https://doi.org/10.3390/jcm10020227
Kholinne E, Lee HJ, Lee YM et al (2018) Mechanoreceptor profile of the lateral collateral ligament complex in the human elbow. Asia-Pacific J Sport Med Arthrosc Rehabil Technol 14:17–21. https://doi.org/10.1016/j.asmart.2018.04.001
Kholinne E, Lee HJ, Kim GY et al (2018) Mechanoreceptors distribution in the human medial collateral ligament of the elbow. Orthop Traumatol Surg Res 104:251–255. https://doi.org/10.1016/j.otsr.2018.01.005
Petrie S, Collins G, Solomonow M et al (1998) Mechanoreceptors in the human elbow ligaments. J Hand Surg Am 23:512–518
Kholinne E, Lee H, Deslivia M et al (2019) Neuroanatomical distribution of sensory receptors in the human elbow joint capsule. Shoulder Elb 11:300–304
Koch B, Kurriger G, Brand RA (1995) Characterisation of the neurosensory elements of the feline cranial cruciate ligament. J Anat 187:353–353
Gómez-Barrena E (1999) Gold chloride technique to study articular innervation. A protocol validated through computer-assisted colorimetry. Histol Histopathol 14:69–79
Soule JD (1962) Direct staining of reticular fibers with gold chloride. Biotech Histochem 37:31–34. https://doi.org/10.3109/10520296209114566
Raunest J, Sager M, Bürgener E (1998) Proprioception of the cruciate ligaments: Receptor mapping in an animal model. Arch Orthop Trauma Surg 118:159–163. https://doi.org/10.1007/s004020050338
Albuerne M, De Lavallina J, Esteban I et al (2000) Development of Meissner-like and Pacinian sensory corpuscles in the mouse demonstrated with specific markers for corpuscular constituents. Anat Rec 258:235–242. https://doi.org/10.1002/(SICI)1097-0185(20000301)258:3%3c235::AID-AR2%3e3.0.CO;2-M
Hagert E, Ljung BO, Forsgren S (2004) General innervation pattern and sensory corpuscles in the scapholunate interosseous ligament. Cells Tissues Organs 177:47–54. https://doi.org/10.1159/000078427
Pederiva F, Aras Lopez R, Martinez L, Tovar JA (2008) Abnormal development of tracheal innervation in rats with experimental diaphragmatic hernia. Pediatr Surg Int 24:1341–1346. https://doi.org/10.1007/s00383-008-2261-2
Rein S, Hagert E, Hanisch U et al (2013) Immunohistochemical analysis of sensory nerve endings in ankle ligaments: A cadaver study. Cells Tissues Organs 197:64–76. https://doi.org/10.1159/000339877
Tingaker BK, Ekman-Ordeberg G, Forsgren S (2006) Presence of sensory nerve corpuscles in the human corpus and cervix uteri during pregnancy and labor as revealed by immunohistochemistry. Reprod Biol Endocrinol 4:1–8. https://doi.org/10.1186/1477-7827-4-45
Lee J, Ladd A, Hagert E (2012) Immunofluorescent triple-staining technique to identify sensory nerve endings in human thumb ligaments. Cells Tissues Organs 195:456–464. https://doi.org/10.1159/000327725
Rein S, Esplugas M, Garcia-Elias M et al (2020) Immunofluorescence analysis of sensory nerve endings in the interosseous membrane of the forearm. J Anat 236:906–915. https://doi.org/10.1111/joa.13138
Robertson D, Savage K, Reis-Filho JS, Isacke CM (2008) Multiple immunofluorescence labelling of formalin-fixed paraffin-embedded (FFPE) tissue. BMC Cell Biol 9:1–10. https://doi.org/10.1186/1471-2121-9-13
Bataille F, Troppmann S, Klebl F et al (2006) Multiparameter immunofluorescence on paraffin-embedded tissue sections. Appl Immunohistochem Mol Morphol 14:225–228. https://doi.org/10.1097/01.pai.0000162009.31931.10
Gesslbauer B, Hruby LA, Roche AD et al (2017) Axonal components of nerves innervating the human arm. Ann Neurol 82:396–408. https://doi.org/10.1002/ana.25018
Zhou X, Du J, Qing L et al (2021) Identification of sensory and motor nerve fascicles by immunofluorescence staining after peripheral nerve injury. J Transl Med 19:1–12. https://doi.org/10.1186/s12967-021-02871-w
Currier SF, Mautner HG (1974) On the mechanism of action of choline acetyltransferase. Proc Nat Acad Sci USA 71:3355–3358. https://doi.org/10.1016/B978-008055232-3.60522-7
Bellier JP, Kimura H (2011) Peripheral type of choline acetyltransferase: Biological and evolutionary implications for novel mechanisms in cholinergic system. J Chem Neuroanat 42:225–235. https://doi.org/10.1016/j.jchemneu.2011.02.005
Sly WS, Hu PY (1995) Human carbonic anhydrases and carbonic anhydrase deficiencies. Annu Rev Biochem 64:375–401. https://doi.org/10.1146/annurev.bi.64.070195.002111
Tashian RE (1992) Genetics of the mammalian carbonic anhydrases. Adv Genet 30:321–356
Carson K, Terzis JK (1985) Carbonic anhydrase histochemistry. A potential dignostic method for peripheral nerve repair. Clin Plast Surg 12:227–232
Riley DA, Lang DH (1984) Carbonic anhydrase activity of human peripheral nerves: A possible histochemical aid to nerve repair. J Hand Surg Am 9:112–120. https://doi.org/10.1016/S0363-5023(84)80198-7
Hewitt SM, Baskin DG, Frevert CW et al (2014) Controls for Immunohistochemistry: The Histochemical Society’s Standards of Practice for Validation of Immunohistochemical Assays. J Histochem Cytochem 62:693–697. https://doi.org/10.1369/0022155414545224
Denti M, Monteleone M, Berardi A, Panni A (1994) Anterior cruciate ligament mechanoreceptors. Histologic studies on lesions and reconstruction. Clin Orthop Relat Res 308:29–32
Krenn V, Morawietz L, Burmester GR et al (2006) Synovitis score: Discrimination between chronic low-grade and high-grade synovitis. Histopathology 49:358–364. https://doi.org/10.1111/j.1365-2559.2006.02508.x
Freeman MAR, Wyke B (1967) The innervation of the ankle joint. An anatomical and histological study in the cat. Acta Anat (Basel) 68:321–333. https://doi.org/10.1159/000143037
Hagert E (2008) Wrist ligaments- innervation patterns and ligamento-muscular reflexes. Thesis for doctoral degree. Karolinska Institutet, Stockholm Sweden. https://openarchive.ki.se/xmlui/bitstream/handle/10616/39802/thesis.pdf?sequence=1&isAllowed=y. Retrieved on 17.08.2022
Hagert E, Garcia-Elias M, Forsgren S, Ljung BO (2007) Immunohistochemical analysis of wrist ligament innervation in relation to their structural composition. J Hand Surg Am 32:30–36. https://doi.org/10.1016/j.jhsa.2006.10.005
Schultz RA, Miller DC, Kerr CS, Micheli L (1984) Mechanoreceptors in human cruciate ligaments: A histological study. J Bone Joint Surg [Br] 66:1072–1976. https://doi.org/10.2106/00004623-198466070-00014
Takebayashi T, Yamashita T, Sakamoto N et al (2002) Biomechanical characteristics of the lateral ligament of the ankle joint. J Foot Ankle Surg 41:154–157. https://doi.org/10.1016/S1067-2516(02)80064-3
Chowdhury R, Matyas JR, Frank CB (1991) The “epiligament” of the rabbit medial collateral ligament: A quantitative morphological study. Connect Tissue Res 27:33–50. https://doi.org/10.3109/03008209109006993
Regan WD, Korinek SL, Morrey BF, An KN (1991) Biomechanical study of ligaments around the elbow joint. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199110000-00023
Kimata K, Yasui M, Yokota H et al (2019) Transverse ligament of the elbow joint: an anatomic study of cadavers. J Shoulder Elb Surg 28:2253–2258. https://doi.org/10.1016/j.jse.2019.04.048
Safran MR, Baillargeon D (2005) Soft-tissue stabilizers of the elbow. J Shoulder Elb Surg 14:S179–S185. https://doi.org/10.1016/j.jse.2004.09.032
O’Discroll S, Bell D, Morrey B (1991) Posterolateral rotatory instability of the elbow. J Bone Jt Surg Am 73:440–446
Jensen AR, LaPrade MD, Turner TW et al (2020) The history and evolution of elbow medial ulnar collateral ligament reconstruction: from Tommy John to 2020. Curr Rev Musculoskelet Med 13:349–360. https://doi.org/10.1007/s12178-020-09618-y
Halata Z, Wagner C, Baumann KI (1999) Sensory nerve endings in the anterior cruciate ligament (Lig. cruciatum anterius) of sheep. Anat Rec 254:13–21. https://doi.org/10.1002/(SICI)1097-0185(19990101)254:1%3c13::AID-AR3%3e3.0.CO;2-4
Ring D, Adey L, Zurakowski D, Jupiter JB (2006) Elbow capsulectomy for posttraumatic elbow stiffness. J Hand Surg Am 31:1264–1271. https://doi.org/10.1016/j.jhsa.2006.06.009
Petrie S, Collins J, Solomonow M et al (1997) Mechanoreceptors in the palmar wrist ligaments. J Bone Joint Surg [Br] 79:494–496. https://doi.org/10.1302/0301-620X.79B3.7439
Callaway GH, Field LD, Deng XH et al (1997) Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg [Br] 79:1223–1231. https://doi.org/10.2106/00004623-199708000-00015
Camp CL, Jahandar H, Sinatro AM et al (2018) Quantitative anatomic analysis of the medial ulnar collateral ligament complex of the elbow. Orthop J Sport Med 6:1–9. https://doi.org/10.1177/2325967118762751
Mioton LM, Dumanian GA, De la Garza M, Ko JH (2019) Histologic analysis of sensory and motor axons in branches of the human brachial plexus. Plast Reconstr Surg 144:1359–1368. https://doi.org/10.1097/PRS.0000000000006278
Xianyu M, Zhenggang B, Laijin L (2016) Identification of the sensory and motor fascicles in the peripheral nerve: A historical review and recent progress. Neurol India 64:880–885. https://doi.org/10.4103/0028-3886.190241
Grigg P, Hoffman A, Fogarty K (1982) Properties of Golgi-Mazzoni afferents in cat knee joint capsule, as revealed by mechanical studies of isolated joint capsule. J Neurophysiol 47:31–40
Grigg P, Hoffman AH (1982) Properties of Ruffini afferents revealed by stress analysis of isolated sections of cat knee capsule. J Neurophysiol 47:41–54
Moore AR, Fleisig GS, Dugas JR (2019) Ulnar collateral ligament repair. Orthop Clin North Am 50:383–389. https://doi.org/10.1016/j.ocl.2019.03.005
Riemann BL, Lephart SM (2002) The sensorimotor system, Part II: The role of proprioception in motor control and functional joint stability. J Athl Train 37:80–84. https://doi.org/10.1016/j.jconhyd.2010.08.009
Riemann BL, Lephart SM (2002) The sensorimotor system, part I: The physiologic basis of functional joint stability. J Athl Train 37:71–79. https://doi.org/10.1016/j.jconhyd.2010.08.009
Wilps T, Kaufmann RA, Yamakawa S, Fowler JR (2020) Elbow biomechanics: bony and dynamic stabilizers. J Hand Surg Am 45:528–535. https://doi.org/10.1016/j.jhsa.2020.01.016
Unal M, Budeyri A, Ercan S et al (2019) Arthroscopic chronic tennis elbow surgery preserves elbow proprioception. Orthop Traumatol Surg Res 105:329–334. https://doi.org/10.1016/j.otsr.2018.10.009
Olsen BS, Søjbjerg JO (2003) The treatment of recurrent posterolateral instability of the elbow. J Bone Joint Surg [Br] 85:342–346. https://doi.org/10.1302/0301-620X.85B3.13669
Savoie FH, O’Brien MJ, Field LD, Gurley DJ (2010) Arthroscopic and open radial ulnohumeral ligament reconstruction for posterolateral rotatory instability of the elbow. Clin Sports Med 29:611–618. https://doi.org/10.1016/j.csm.2010.06.008
Cohen MS, Hastings H (1995) Rotatory instability of the elbow: The lateral stabilizers. J Shoulder Elb Surg 4:S10. https://doi.org/10.1016/s1058-2746(95)80049-2
Reichel LM, Milam GS, Sitton SE et al (2013) Elbow lateral collateral ligament injuries. J Hand Surg Am 38:184–201. https://doi.org/10.1016/j.jhsa.2012.10.030
Wilhelm A (2000) Die Denervation zur Behandlung der therapieresistenten Epicondylitis humeri lateralis. Oper Orthop Traumatol 12:95–108
Bellato E, Castoldi F, Marmotti A et al (2020) Relationship between the lateral collateral ligament of the elbow and the Kocher approach: A cadaver study. J Hand Surg Am. https://doi.org/10.1016/j.jhsa.2020.09.013
Weiss APC, Hastings H (1992) The anatomy of the proximal radioulnar joint. J Shoulder Elb Surg 1:193–199. https://doi.org/10.1016/1058-2746(92)90013-S
Kim MC, Eckhardt BP, Craig C, Kuhns LR (2004) Ultrasonography of the annular ligament partial tear and recurrent “pulled elbow.” Pediatr Radiol 34:999–1004. https://doi.org/10.1007/s00247-004-1284-7
Tan JW, Mu MZ, Liao GJ, Li JM (2008) Pathology of the annular ligament in paediatric Monteggia fractures. Injury 39:451–455. https://doi.org/10.1016/j.injury.2007.07.010
Cheung E, Nathani A, Tashjian R et al (2019) Elbow trauma sequelae: instability, stiffness, non-arthroplasty, and arthroplasty options. Instr Course Lect 68:117–140
Wilhelm A (1958) Zur Innervation der Gelenke der oberen Extremität. Z Anat Entwicklungsgesch 120:331–371. https://doi.org/10.1007/BF00525089
Laumonerie P, Tiercelin J, Tibbo ME et al (2020) Sensory innervation of the human elbow joint and surgical considerations. Clin Anat 33:1062–1068. https://doi.org/10.1002/ca.23538
Acknowledgements
We thank Manuel Llusa, MD, PhD (Department of Anatomy, University of Barcelona, Barcelona, Spain) for generous assistance in the laboratory work. We thank the BioImaging Core Facility BCF (http://www.maginlab.eu/home-bcf.html).
Funding
This study has been financially supported by Deutsche Gesetzliche Unfallversicherung, Sankt Augustin, Germany (grant number: FR-0272) and Bauerfeind AG, Zeulenroda-Triebes, Germany (grant number: 8344). The authors disclose any financial conflicts of interest that may influence interpretation of this study and/ or results.
Author information
Authors and Affiliations
Contributions
All authors made substantive intellectual contributions to this study, in conception and design (SR, ME, MGE, FS), acquisition of data (SR, ME, MGE, PL), analysis and interpretation of data (SR, FS, PL), drafting and revising the manuscript (SR, ME, MGE, TK, FS, PL), as well as final approval of the version to be submitted (SR, ME, MGE, TK, FS, PL). All authors have read and approved the final submitted manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests. This study has been financially supported by Deutsche Gesetzliche Unfallversicherung, Sankt Augustin, Germany (grant number: FR-0272) and Bauerfeind AG, Zeulenroda-Triebes, Germany (grant number: 8344). The authors disclose any financial conflicts of interest that may influence interpretation of this study and/ or results.
Ethical approval
All protocols in this study were approved by the local ethics committee review board (approval number 33/17).
Informed consent
The present study is a cadaver study, therefore no informed consent had to be obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rein, S., Esplugas, M., Garcia-Elias, M. et al. Immunofluorescence analysis of sensory nerve endings in the periarticular tissue of the human elbow joint. Arch Orthop Trauma Surg 143, 3779–3794 (2023). https://doi.org/10.1007/s00402-022-04604-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04604-0