Abstract
Introduction
High body mass index (BMI) and wound drainage following total joint arthroplasty (TJA) can lead to wound healing complications and periprosthetic joint infection. Silver-embedded occlusive dressings and negative pressure wound therapy (NPWT) have been shown to reduce these complications. The purpose of this prospective trial was to compare the effect of silver-embedded dressings and NPWT on wound complications in patients with BMI ≥ 35 m/kg2 undergoing TJA.
Methods
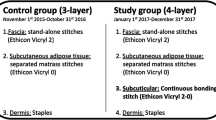
We conducted a randomized control trial of patients who had a BMI > 35 m/kg2 and were undergoing primary TJA between October 2017 and February 2020. Patients who underwent revision surgery, or those with an active infection, previous scar, history of wound healing complications, post-traumatic degenerative joint disease with hardware, or inflammatory arthritis were excluded. Patients were randomized to receive either a silver-embedded occlusive dressing (control) or NPWT. Frequency distributions, means, and standard deviations were used to describe patient demographics, postoperative complications, 90-day readmissions, and reoperations. T-test and chi-squared tests were used to test for significant differences between continuous and categorical variables, respectively.
Results
Two hundred-thirty patients with 3-month follow-up were included. One-hundred-fifteen patients received the control and 115 patients received NPWT. There were six patients (5.2%) in the control group with wound complications (drainage: n = 5, non-healing wound: n = 1) and two patients (1.7%) in the NPWT with complications (drainage: n = 2). There were no 90-day readmissions in the control group versus two (1.8%) 90-day readmissions in the NPWT group. Finally, three patients (2.6%) in the control group underwent reoperations (irrigation and debridement [I&D], I&D with modular implant exchange, and implant revision), while none in the NPWT group had undergone reoperation. The two groups showed insignificant differences in wound complications (p = 0.28), 90-day readmissions (p = 0.50), and reoperations (p = 0.25).
Conclusion
Patients with BMI ≥ 35 m/kg2 undergoing TJA have no statistical difference in early wound complications, readmissions, or reoperations when treated with either silver-embedded dressings or NPWT.
Similar content being viewed by others
Change history
12 November 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00402-022-04691-z
17 July 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00402-022-04552-9
References
Grayson CW, Decker RC (2012) Total joint arthroplasty for persons with osteoarthritis. PM R 4:97–103. https://doi.org/10.1016/j.pmrj.2012.02.018
Anderson JJ, Felson DT (1988) Factors associated with osteoarthritis of the knee in the first national health and nutrition examination survey (hanes i): evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol 128:179–189. https://doi.org/10.1093/oxfordjournals.aje.a114939
Oliveria SA, Felson DT, Cirillo PA, Reed JI, Walker AM (1999) Body weight, body mass index, and incident symptomatic osteoarthritis of the hand, hip, and knee. Epidemiology. https://doi.org/10.1097/00001648-199903000-00013
Pottie P, Presle N, Terlain B et al (2006) Obesity and osteoarthritis: more complex than predicted! Ann Rheum Dis 65:1403–1405. https://doi.org/10.1136/ard.2006.061994
Meller MM, Toossi N, Johanson NA et al (2016) Risk and cost of 90-day complications in morbidly and superobese patients after total knee arthroplasty. J Arthroplasty 31:2091–2098. https://doi.org/10.1016/j.arth.2016.02.062
Watts CD, Houdek MT, Wagner ER, Taunton MJ (2016) Subcutaneous fat thickness is associated with early reoperation and infection after total knee arthroplasty in morbidly obese patients. J Arthroplasty 31:1788–1791. https://doi.org/10.1016/j.arth.2016.02.008
Yu S, Siow M, Odeh K et al (2018) Periarticular soft tissue envelope size and postoperative wound complications following total knee arthroplasty. J Arthroplasty 33:S249–S252. https://doi.org/10.1016/j.arth.2018.02.046
Jämsen E, Nevalainen P, Eskelinen A et al (2012) Obesity, diabetes, and preoperative hyperglycemia as predictors of periprosthetic joint infection: a single-center analysis of 7181 primary hip and knee replacements for osteoarthritis. J Bone Jt Surg - Ser A 94:e101. https://doi.org/10.2106/JBJS.J.01935
Malinzak RA, Ritter MA, Berend ME et al (2009) Morbidly obese, diabetic, younger, and unilateral joint arthroplasty patients have elevated total joint arthroplasty infection rates. J Arthroplasty 24:84–88. https://doi.org/10.1016/j.arth.2009.05.016
Hebert CK, Williams RE, Levy RS, Barrack RL (1996) Cost of treating an infected total knee replacement. Clin Orthop Relat Res 331:140–145. https://doi.org/10.1097/00003086-199610000-00019
Okafor C, Hodgkinson B, Nghiem S et al (2021) Cost of septic and aseptic revision total knee arthroplasty: a systematic review. BMC Musculoskelet Disord 22:1–14. https://doi.org/10.1186/s12891-021-04597-8
Springer BD, Beaver WB, Griffin WL et al (2015) Role of surgical dressings in total joint arthroplasty: a randomized controlled trial. Am J Orthop (Belle Mead NJ) 44:415–420
Darouiche RO (2004) Treatment of infections associated with surgical implants. N Engl J Med 350:1422–1429. https://doi.org/10.1056/NEJMra035415
Cai J, Karam JA, Parvizi J et al (2014) Aquacel surgical dressing reduces the rate of acute PJI following total joint arthroplasty: a case-control study. J Arthroplasty 29:1098–1100. https://doi.org/10.1016/j.arth.2013.11.012
Karlakki SL, Hamad AK, Whittall C et al (2016) Incisional negative pressure wound therapy dressings (inpWTd) in routine primary hip and knee arthroplasties: a randomised controlled trial. Bone Jt Res 5:328–337. https://doi.org/10.1302/2046-3758.58.BJR-2016-0022.R1
Cooper HJ, Bas MA (2016) Closed-incision negative-pressure therapy versus antimicrobial dressings after revision hip and knee surgery: a comparative study. J Arthroplasty 31:1047–1052. https://doi.org/10.1016/j.arth.2015.11.010
Grosso MJ, Berg A, LaRussa S et al (2017) Silver-impregnated occlusive dressing reduces rates of acute periprosthetic joint infection after total joint arthroplasty. J Arthroplasty 32:929–932. https://doi.org/10.1016/j.arth.2016.08.039
Vasconcelos A, Cavaco-Paulo A (2011) Wound dressings for a proteolytic-rich environment. Appl Microbiol Biotechnol 90:445–460. https://doi.org/10.1007/s00253-011-3135-4
Keeney JA, Cook JL, Clawson SW et al (2019) Incisional negative pressure wound therapy devices improve short-term wound complications, but not long-term infection rate following hip and knee arthroplasty. J Arthroplasty 34:723–728. https://doi.org/10.1016/j.arth.2018.12.008
Kim PJ, Attinger CE, Constantine T et al (2020) Negative pressure wound therapy with instillation: international consensus guidelines update. Int Wound J 17:174–186. https://doi.org/10.1111/iwj.13254
Doman DM, Young AM, Buller LT et al (2021) Comparison of surgical site complications with negative pressure wound therapy vs silver impregnated dressing in high-risk total knee arthroplasty patients: a matched cohort study. J Arthroplasty 36:3437–3442. https://doi.org/10.1016/j.arth.2021.05.030
Higuera-Rueda CA, Emara AK, Nieves-Malloure Y et al (2021) The effectiveness of closed-incision negative-pressure therapy versus silver-impregnated dressings in mitigating surgical site complications in high-risk patients after revision knee arthroplasty: the PROMISES randomized controlled trial. J Arthroplasty 36:S295-S302e14. https://doi.org/10.1016/j.arth.2021.02.076
Newman JM, Siqueira MBP, Klika AK et al (2019) Use of closed incisional negative pressure wound therapy after revision total hip and knee arthroplasty in patients at high risk for infection: a prospective, randomized clinical trial. J Arthroplasty 34:554-559.e1. https://doi.org/10.1016/j.arth.2018.11.017
Wang L, Xu X, Cao J, Liu J (2019) Negative pressure wound therapy in total hip and knee arthroplasty: a meta-analysis. J Comp Eff Res 8:791–797. https://doi.org/10.2217/cer-2019-0009
Kuo F-C, Hsu C-W, Tan TL et al (2021) Effectiveness of different wound dressings in the reduction of Blisters and Periprosthetic joint infection after total joint arthroplasty: a systematic review and network meta-analysis. J Arthroplasty 36:2612–2629. https://doi.org/10.1016/j.arth.2021.02.047
Chowdhry M, Chen AF (2015) Wound dressings for primary and revision total joint arthroplasty. Ann Transl Med 3:1–7. https://doi.org/10.3978/j.issn.2305-5839.2015.09.25
Ravenscroft M, Harker J, Buch K (2006) A prospective, randomised, controlled trial comparing wound dressings used in hip and knee surgery: Aquacel and Tegaderm versus Cutiplast. Ann R Coll Surg Engl 88:18–22. https://doi.org/10.1308/003588406X82989
Gupta SK, Lee S, Moseley LG (2002) Postoperative wound blistering: is there a link with dressing usage? J Wound Care 11:271–273. https://doi.org/10.12968/jowc.2002.11.7.26413
Cosker T, Elsayed S, Gupta S et al (2005) Choice of dressing has a major impact on blistering and healing outcomes in orthopaedic patients. J Wound Care 14:27–29. https://doi.org/10.12968/jowc.2005.14.1.26722
Funding
This research received no external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors 1, 2, 3, and 4 have no conflict of interests to disclose. Author 5 owns stock or stock options in Intellijoint, Gauss surgical, and PSI. Author 5 is a paid consultant for Smith & Nephew and Intellijoint. Author 5 is also on the editorial/governing board for the Journal of Arthroplasty and Arthroplasty Today and is a board member for AAOS and AAHKS. Author 6 is a paid consultant/speaker for Convatec, DePuy, Pacira, Think Surgical, and TJO. Author 6 has received royalties from Elsevier and OrthoDevelopment. Author 6 is also on the editorial/governing board of the Journal of Arthroplasty and is a board member for AAOS.
Ethical approval
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of NYU School of Medicine (study number: i17-00496_CR2).
Informed consent
All subjects gave their informed consent for inclusion before they participated in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lygrisse, K.A., Teo, G., Singh, V. et al. Comparison of silver-embedded occlusive dressings and negative pressure wound therapy following total joint arthroplasty in high BMI patients: a randomized controlled trial. Arch Orthop Trauma Surg 143, 2989–2995 (2023). https://doi.org/10.1007/s00402-022-04530-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04530-1