Abstract
Introduction
Prior studies of hamstring tendon tears have reported varied findings on whether increased delay from injury to surgery is associated with worse outcomes. The purpose of this study was to determine whether increased time from injury to surgical repair is associated with worse clinical outcomes in patients with proximal hamstring ruptures.
Materials and methods
Patients who underwent surgical repair of a proximal hamstring rupture from 2010 to 2019 were followed for a minimum of 24 months from surgery. A cutoff of 6 weeks from injury to the time of surgery was used to distinguish between acute and chronic ruptures. All patients completed patient-reported outcome measures (PROs) at the final follow-up. Multiple factors were analyzed for their effects on PROs including time to surgery, amount of tendon retraction, and demographics such as sex and age.
Results
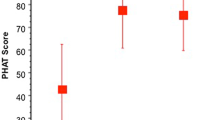
Complete data sets were obtained for 38 patients at a mean follow-up of 4.9 years. All data is reported as a mean ± standard deviation. Patients who underwent acute repair of proximal hamstring ruptures had significantly greater Perth Hamstring Assessment Tool (PHAT) scores than those who underwent chronic repair (76.9 ± 18.8 vs 60.6 ± 18.2, p = 0.01). Increased time to surgery was significantly correlated with worse PHAT scores (ρ = − 0.47, p = 0.003). There was no difference in PROs based on the amount of tendon retraction, number of tendons torn, sex, smoking status, or BMI.
Conclusions
This study found that acute repair performed within 6 weeks of injury appears to yield improved PROs compared to chronic repair. These data highlight the importance of timely and accurate diagnosis of proximal hamstring ruptures and early operative intervention for surgical candidates.
Similar content being viewed by others
Abbreviations
- PEEK:
-
Polyether Ether Ketone
- PRO:
-
Patient Reported Outcome
- PHAT:
-
Perth Hamstring Assessment Tool
- MHHS:
-
Modified Harris Hip Score
- VAS:
-
Visual Analogue Scale for Pain
References
Irger M, Willinger L, Lacheta L, Pogorzelski J, Imhoff AB, Feucht MJ (2020) Proximal hamstring tendon avulsion injuries occur predominately in middle-aged patients with distinct gender differences: epidemiologic analysis of 263 surgically treated cases. Knee Surg Sports Traumatol Arthrosc 28(4):1221–1229
van der Made AD, Tol JL, Reurink G, Peters RW, Kerkhoffs GM (2019) Potential hamstring injury blind spot: we need to raise awareness of proximal hamstring tendon avulsion injuries. Br J Sports Med 53(7):390–392
Piposar JR, Vinod AV, Olsen JR, Lacerte E, Miller SL (2017) High-grade partial and retracted (< 2 cm) proximal hamstring ruptures: nonsurgical treatment revisited. Orthop J Sports Med 5(2):2325967117692507
Bodendorfer BM, Curley AJ, Kotler JA et al (2018) outcomes after operative and nonoperative treatment of proximal hamstring avulsions: a systematic review and meta-analysis. Am J Sports Med 46(11):2798–2808
Shambaugh BC, Olsen JR, Lacerte E, Kellum E, Miller SL (2017) A comparison of nonoperative and operative treatment of complete proximal hamstring ruptures. Orthop J Sports Med 5(11):2325967117738551
Wood D, French SR, Munir S, Kaila R (2020) The surgical repair of proximal hamstring avulsions: does the timing of surgery or injury classification influence long-term patient outcomes? Bone Joint J 102(10):1419–1427
Van Der Made AD, Reurink G, Gouttebarge V, Tol JL, Kerkhoffs GM (2015) Outcome after surgical repair of proximal hamstring avulsions: a systematic review. Am J Sports Med 43(11):2841–2851
Léger-St-Jean B, Gorica Z, Magnussen RA, Vasileff WK, Kaeding CC (2019) Accelerated rehabilitation results in good outcomes following acute repair of proximal hamstring ruptures. Knee Surg Sports Traumatol Arthrosc 27(10):3121–3124
Rust DA, Giveans MR, Stone RM, Samuelson KM, Larson CM (2014) Functional outcomes and return to sports after acute repair, chronic repair, and allograft reconstruction for proximal hamstring ruptures. Am J Sports Med 42(6):1377–1383
Blakeney WG, Zilko SR, Edmonston SJ, Schupp NE, Annear PT (2017) Proximal hamstring tendon avulsion surgery: evaluation of the Perth Hamstring Assessment Tool. Knee Surg Sports Traumatol Arthrosc 25(6):1936–1942
Ovre S, Sandvik L, Madsen JE, Roise O (2007) Modification of the Harris Hip Score in acetabular fracture treatment. Injury 38(3):344–349
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Akoglu H (2018) User’s guide to correlation coefficients. Turk J Emerg Med 18(3):91–93
Best R, Eberle J, Beck F, Huth J, Becker U (2017) Surgical refixation after proximal hamstring tendon avulsion injuries: does the time of surgery influence functional outcomes? Sportverletz Sportschaden 31(3):160–166
Blakeney WG, Zilko SR, Edmonston SJ, Schupp NE, Annear PT (2017) A prospective evaluation of proximal hamstring tendon avulsions: improved functional outcomes following surgical repair. Knee Surg Sports Traumatol Arthrosc 25(6):1943–1950
Shambaugh BC, Wuerz TH, Miller SL (2020) Does Time From Injury to Surgery Affect Outcomes After Surgical Repair of Partial and Complete Proximal Hamstring Ruptures? Orthop J Sports Med, 8(8):2325967120946317
Thomsen NO, Jensen TT (1999) Late repair of rupture of the hamstring tendons from the ischial tuberosity-a case report. Acta Orthop Scand 70(1):89–91
Subbu R, Benjamin-Laing H, Haddad F (2015) Timing of surgery for complete proximal hamstring avulsion injuries: successful clinical outcomes at 6 weeks, 6 months, and after 6 months of injury. Am J Sports Med 43(2):385–391
Birmingham P, Muller M, Wickiewicz T, Cavanaugh J, Rodeo S, Warren R (2011) Functional outcome after repair of proximal hamstring avulsions. J Bone Joint Surg 93(19):1819–1826
Willinger L, Siebenlist S, Lacheta L et al (2020) Excellent clinical outcome and low complication rate after proximal hamstring tendon repair at mid-term follow up. Knee Surg Sports Traumatol Arthrosc 28(4):1230–1235
Cohen S, Bradley J (2007) Acute proximal hamstring rupture. J Am Acad Orthop Surg 15(6):350–355
Pasic N, Giffin JR, Degen RM (2020) Practice patterns for the treatment of acute 416 proximal hamstring ruptures. Phys Sportsmed, 48(1):116-122
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Thomas Youm is a paid consultant for Arthrex. Laith Jazrawi is a member of the editorial or governing board for Bulleting to the Hospital for Joint Diseases and JBJS Reviews, receives publishing royalties from Wolters Kluwers Health—Lippincott Williams & Wilkins, and receives research support from Arthrex, Smith & Nephew, and Mitek. None of these disclosures are relevant to the current work, and no industry or other external support was provided for this study. The authors declare no other potential conflicts of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors. IRB approval (i20-00889) was obtained prior to commencing the study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kanakamedala, A.C., Mojica, E.S., Hurley, E.T. et al. Increased time from injury to surgical repair in patients with proximal hamstring ruptures is associated with worse clinical outcomes at mid-term follow-up. Arch Orthop Trauma Surg 143, 951–957 (2023). https://doi.org/10.1007/s00402-022-04421-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04421-5