Abstract
Introduction
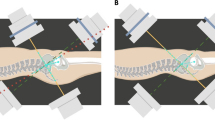
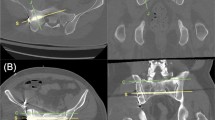
Between 2005 and 2017, the number of closed reduction and internal fixation of pelvic ring injuries increased by 1116%. Percutaneous fixation is currently the only minimally invasive technique that can stabilize the posterior elements of the pelvis. The purpose of this study was to investigate the utility of the inlet obturator oblique view (IOO) with the hypothesis that the IOO view will improve the accuracy of sacroiliac and transsacral screw placement in the S1 or S2 body and improve the accuracy of assessing whether the implant is fully seated against the outer cortex of the ilium.
Materials and methods
Ten male pelvic training models were used. Thirty-six screw configurations were inserted by a fellowship trained orthopedic trauma surgeon in appropriately and inappropriately placed sacroiliac and transsacral screw configurations. These configurations were imaged using fluoroscopy in different planes and saved for survey.
Results
Fourteen orthopedic professionals reviewed 313 fluoroscopic images. Interrater reliability demonstrated marked improvement in assessment of whether the screw head was seated against the outer cortex of the ilium with the IOO view (kappa = 0.841, without IOO kappa = 0.027). There was a statistically significant difference in overall accuracy (p value < 0.001, OR = 1.57, 95% CI = 1.35–1.84) and whether the screw head was seated (p value < 0.001, OR = 8.14, 95% CI = 5.52–11.99) when compared with and without the IOO view (accuracy with IOO view: 85%, accuracy without IOO view: 78.26%; screw seated with IOO view: 93.93%, screw seated without IOO view: 65.54%). There was no significant difference (p value 0.465, OR = 1.13, 95% CI = 0.82–1.55) determining if the screw was in a safe position (safe with IOO view: 84.64%, safe without IOO view: 83.04%).
Conclusions
Our findings demonstrate that misinterpretation of sacroiliac and transsacral screw placement can occur with the standard fluoroscopic imaging. We suggest the addition of the IOO view increases the overall accuracy of screw placement and whether the screw head is fully seated against the outer table of the ilium. This in turn can improve fixation and potentially improve patient outcomes and decrease adverse events.






Similar content being viewed by others
Change history
12 March 2022
Author’s personal address is listed next to the hospital name instead of the hospital address. The hospital address is 26520 Cactus Ave, Moreno Valley, CA 92555
References
Lodde M, Katthagen C, Riesenbeck O, Raschke M, Hartensuer R (2021) Trends in the surgical treatment of fractures of the pelvic ring: a nationwide analysis of operations and procedure code (OPS) data between 2005 and 2017. Unfallchirurg 124(5):373–381
Smith HE, Yuan PS, Sasso R, Papadopolous S, Vaccaro AR (2006) An evaluation of image-guided technologies in the placement of percutaneous iliosacral screws. Spine 31(2):234–238
Pizanis A, Pohlemann T, Burkhardt M, Aghayev E, Holstein JH (2013) Emergency stabilization of the pelvic ring: clinical comparison between three different techniques. Injury 44(12):1760–1764
Alvis-miranda HR, Farid-escorcia H, Alcalá-cerra G, Castellar-leones SM, Moscote-salazar LR (2014) Sacroiliac screw fixation: a mini review of surgical technique. J Craniovertebr Junction Spine 5(3):110–113
Zwingmann J, Hauschild O, Bode G, Südkamp NP, Schmal H (2013) Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: a systematic review and meta-analysis. Arch Orthop Trauma Surg 133(9):1257–1265
Tonetti J, Carrat L, Blendea S et al (2001) Clinical results of percutaneous pelvic surgery. Computer assisted surgery using ultrasound compared to standard fluoroscopy. Comput Aided Surg 6(4):204–211
Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P (2005) Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am 87-A:260–267
Landis JR, Koch GG (1997) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Altman DG (1999) Practical statistics for medical research. Chapman & Hall/CRC Press, New York
Routt ML, Nork SE, Mills WJ (2000) Percutaneous fixation of pelvic ring disruptions. Clin Orthop Relat Res 375:15–29
Van den Bosch EW, Van Zwienen CM, Van Vugt AB (2002) Fluoroscopic positioning of sacroiliac screws in 88 patients. J Trauma 53(1):44–48
Guimarães JAM, Martin MP, Da Silva FR et al (2019) The obturator oblique and iliac oblique/outlet views predict most accurately the adequate position of an anterior column acetabular screw. Int Orthop 43(5):1205–1213
Starr AJ, Walter JC, Harris RW, Reinert CM, Jones AL (2002) Percutaneous screw fixation of fractures of the iliac wing and fracture-dislocations of the sacro-iliac joint (OTA Types 61–B2.2 and 61–B2.3, or Young-Burgess "lateral compression type II" pelvic fractures). J Orthop Trauma 16(2):116–123
Hasenboehler EA, Stahel PF, Williams A et al (2011) Prevalence of sacral dysmorphia in a prospective trauma population: implications for a “safe” surgical corridor for sacro-iliac screw placement. Patient Saf Surg 5(1):8
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors whose names are listed directly above certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained by each participant who took part in completing the survey.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barger, K., Robinson, M. An evaluation of the inlet obturator oblique view for sacroiliac and transsacral screw placement. Arch Orthop Trauma Surg 143, 1869–1875 (2023). https://doi.org/10.1007/s00402-022-04370-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04370-z