Abstract
Introduction
Systemically, changes in serum platelet to lymphocyte ratio (PLR), platelet count to mean platelet volume ratio (PVR), neutrophil to lymphocyte ratio (NLR) and monocyte to lymphocyte (MLR) represent primary responses to early inflammation and infection. This study aimed to determine whether PLR, PVR, NLR, and MLR can be useful in diagnosing periprosthetic joint infection (PJI) in total hip arthroplasty (THA) patients.
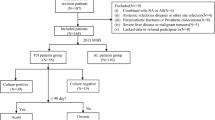
Methods
A total of 464 patients that underwent revision THA with calculable PLR, PVR, NLR, and MLR in 2 groups was evaluated: 1) 191 patients with a pre-operative diagnosis of PJI, and 2) 273 matched patients treated for revision THA for aseptic complications.
Results
The sensitivity and specificity of PLR combined with erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), synovial white blood cell count (WBC) and synovial polymorphonuclear leukocytes (PMN) (97.9%; 98.5%) is significantly higher than only ESR combined with CRP, synovial WBC and synovial PMN (94.2%; 94.5%; p < 0.01). The sensitivity and specificity of PVR combined with ESR, CRP and synovial WBC, and synovial PMN (98.4%; 98.2%) is higher than only ESR combined with CRP, synovial WBC and synovial PMN (94.2%; 94.5%; p < 0.01).
Conclusion
The study results demonstrate that both PLR and PVR calculated from complete blood counts when combined with serum and synovial fluid markers have increased diagnostic sensitivity and specificity in diagnosing periprosthetic joint infection in THA patients.
Level of evidence:III, case–control retrospective analysis.


Similar content being viewed by others
References
Kurtz S, Ong K, Lau E et al (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89:780–785. https://doi.org/10.2106/JBJS.F.00222
Elmallah RK, Chughtai M, Khlopas A et al (2018) Pain control in total knee arthroplasty. J Knee Surg 31:504–513. https://doi.org/10.1055/s-0037-1604152
Arauz P, Klemt C, Limmahakhun S, et al (2018) Stair Climbing and High Knee Flexion Activities in Bi-Cruciate Retaining Total Knee Arthroplasty: In Vivo Kinematics and Articular Contact Analysis. J Arthroplasty. https://doi.org/10.1016/j.arth.2018.11.013
Bourne RB, Chesworth BM, Davis AM et al (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63. https://doi.org/10.1007/s11999-009-1119-9
Klemt C, Tirumala V, Smith EJ et al (2020) Development of a preoperative risk calculator for re-infection following revision surgery for periprosthetic joint infection. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.08.004
George DA, Konan S, Haddad FS (2015) Single-Stage Hip and Knee Exchange for Periprosthetic Joint Infection. J Arthroplasty 30:2264–2270. https://doi.org/10.1016/j.arth.2015.05.047
Klemt C, Tirumala V, Oganesyan R et al (2020) Single-stage revision of the infected total knee arthroplasty is associated with improved functional outcomes: A Propensity Score Matched Cohort Study. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.07.012
Klemt C, Tirumala V, Smith EJ et al (2021) Development of a preoperative risk calculator for reinfection following revision surgery for periprosthetic joint infection. J Arthroplasty 36:693–699. https://doi.org/10.1016/j.arth.2020.08.004
Parvizi J, Tan TL, Goswami K et al (2018) The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria. J Arthroplasty 33:1309-1314.e2. https://doi.org/10.1016/j.arth.2018.02.078
Bernard L, Lubbeke A, Stern R et al (2004) Value of preoperative investigations in diagnosing prosthetic joint infection: retrospective cohort study and literature review. Scand J Infect Dis 36:410–416. https://doi.org/10.1080/00365540410015240
Carli AV, Abdelbary H, Ahmadzai N et al (2019) Diagnostic accuracy of serum, synovial, and tissue testing for chronic periprosthetic joint infection after hip and knee replacements: a systematic review. J Bone Joint Surg Am 101:635–649. https://doi.org/10.2106/JBJS.18.00632
Shahi A, Kheir MM, Tarabichi M et al (2017) Serum D-Dimer test is promising for the diagnosis of periprosthetic joint infection and timing of reimplantation. J Bone Joint Surg Am 99:1419–1427. https://doi.org/10.2106/JBJS.16.01395
Wyatt MC, Beswick AD, Kunutsor SK et al (2016) The alpha-defensin immunoassay and leukocyte esterase colorimetric strip test for the diagnosis of periprosthetic infection: a systematic review and meta-analysis. J Bone Joint Surg Am 98:992–1000. https://doi.org/10.2106/JBJS.15.01142
Sigmund IK, Holinka J, Gamper J, et al (2017) Qualitative alpha-defensin test (Synovasure) for the diagnosis of periprosthetic infection in revision total joint arthroplasty. Bone Joint J 99-B:66–72. https://doi.org/10.1302/0301-620X.99B1.BJJ-2016-0295.R1
Paziuk T, Rondon AJ, Goswami K et al (2019) A novel adjunct indicator of periprosthetic joint infection: platelet count and mean platelet volume. J Arthroplasty. https://doi.org/10.1016/j.arth.2019.10.012
Tirumala V, Klemt C, Xiong L et al (2020) Diagnostic utility of platelet count/lymphocyte count ratio and platelet count/mean platelet volume ratio in periprosthetic joint infection following total knee arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.07.038
Kim NY, Chun D-H, Kim SY et al (2019) Prognostic value of systemic inflammatory indices, NLR, PLR, and MPV, for predicting 1-year survival of patients undergoing cytoreductive surgery with HIPEC. J Clin Med. https://doi.org/10.3390/jcm8050589
Ahsen A, Ulu MS, Yuksel S et al (2013) As a new inflammatory marker for familial Mediterranean fever: neutrophil-to-lymphocyte ratio. Inflammation 36:1357–1362. https://doi.org/10.1007/s10753-013-9675-2
Uslu AU, Deveci K, Korkmaz S et al (2013) Is neutrophil/lymphocyte ratio associated with subclinical inflammation and amyloidosis in patients with familial Mediterranean fever? Biomed Res Int 2013:185317. https://doi.org/10.1155/2013/185317
Erre GL, Paliogiannis P, Castagna F et al (2019) Meta-analysis of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio in rheumatoid arthritis. Eur J Clin Invest 49:e13037. https://doi.org/10.1111/eci.13037
Gasparyan AY, Ayvazyan L, Mukanova U et al (2019) The Platelet-to-lymphocyte ratio as an inflammatory marker in rheumatic diseases. Ann Lab Med 39:345–357. https://doi.org/10.3343/alm.2019.39.4.345
Gao K, Zhu W, Liu W et al (2019) Diagnostic value of the blood monocyte-lymphocyte ratio in knee osteoarthritis. J Int Med Res 47:4413–4421. https://doi.org/10.1177/0300060519860686
Xiang J, Zhou L, Li X et al (2017) Preoperative monocyte-to-lymphocyte ratio in peripheral blood predicts stages, metastasis, and histological grades in patients with ovarian cancer. Transl Oncol 10:33–39. https://doi.org/10.1016/j.tranon.2016.10.006
Vulliamy P, McCluney S, Mukherjee S et al (2016) Postoperative elevation of the neutrophil: lymphocyte ratio predicts complications following esophageal resection. World J Surg 40:1397–1403. https://doi.org/10.1007/s00268-016-3427-z
McNally M, Sousa R, Wouthuyzen-Bakker M, et al (2020) The EBJIS definition of periprosthetic joint infection. Bone Joint J 103-B:18–25. https://doi.org/10.1302/0301-620X.103B1.BJJ-2020-1381.R1
Fan Y, Xiao Y, Sabuhi WA et al (2019) Longitudinal model of periprosthetic joint infection in the rat. J Orthop Res Off Publ Orthop Res Soc. https://doi.org/10.1002/jor.24556
Aron ZD, Mehrani A, Hoffer ED et al (2021) trans-Translation inhibitors bind to a novel site on the ribosome and clear Neisseria gonorrhoeae in vivo. Nat Commun 12:1799. https://doi.org/10.1038/s41467-021-22012-7
Yang Q, Zhang P, Wu R et al (2018) Identifying the best marker combination in CEA, CA125, CY211, NSE, and SCC for lung cancer screening by combining ROC curve and logistic regression analyses: is it feasible? Dis Markers 2018:2082840. https://doi.org/10.1155/2018/2082840
Nosrati M, Dey D, Mehrani A et al (2019) Functionally critical residues in the aminoglycoside resistance-associated methyltransferase RmtC play distinct roles in 30S substrate recognition. J Biol Chem 294:17642–17653. https://doi.org/10.1074/jbc.RA119.011181
Mendez JH, Mehrani A, Randolph P, Stagg S (2019) Throughput and resolution with a next-generation direct electron detector. IUCrJ 6:1007–1013. https://doi.org/10.1107/S2052252519012661
Jafari SM, Coyle C, Mortazavi SMJ et al (2010) Revision hip arthroplasty: infection is the most common cause of failure. Clin Orthop Relat Res 468:2046–2051. https://doi.org/10.1007/s11999-010-1251-6
Kwon Y-M, Mahajan J, Tirumala V et al (2020) Sensitivity and Specificity of Serum and Synovial Fluid Markers in Diagnosis of Infection in Head-Neck Taper Corrosion of Metal-On-Polyethylene Total Hip Arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.06.058
Klemt C, Padmanabha A, Esposito JG, et al Elevated ESR and CRP Prior to Second-Stage Reimplantation Knee Revision Surgery for Periprosthetic Joint Infection Are Associated with Increased Reinfection Rates. J Knee Surg
Riccio G, Cavagnaro L, Akkouche W et al (2018) Qualitative alpha-defensin versus the main available tests for the diagnosis of periprosthetic Joinfile:///Users/christian/Downloads/bandj_bjj103-B_1534.rist infection: best predictor test? J bone Jt Infect 3:156–164. https://doi.org/10.7150/jbji.26401
Saleh A, George J, Faour M et al (2018) Serum biomarkers in periprosthetic joint infections. Bone Joint Res 7:85–93. https://doi.org/10.1302/2046-3758.71.BJR-2017-0323
Bonanzinga T, Zahar A, Dütsch M et al (2017) How reliable is the alpha-defensin immunoassay test for diagnosing periprosthetic joint infection? a prospective study. Clin Orthop Relat Res 475:408–415. https://doi.org/10.1007/s11999-016-4906-0
Unsal E, Aksaray S, Koksal D, Sipit T (2005) Potential role of interleukin 6 in reactive thrombocytosis and acute phase response in pulmonary tuberculosis. Postgrad Med J 81:604–607. https://doi.org/10.1136/pgmj.2004.030544
Malpani R, Haynes MS, Clark MG et al (2019) Abnormally high, as well as low, preoperative platelet counts correlate with adverse outcomes and readmissions after elective total knee arthroplasty. J Arthroplasty 34:1670–1676. https://doi.org/10.1016/j.arth.2019.04.012
Klim SM, Amerstorfer F, Gruber G et al (2018) Fibrinogen - a practical and cost efficient biomarker for detecting periprosthetic joint infection. Sci Rep 8:8802. https://doi.org/10.1038/s41598-018-27198-3
Yao C, Zhang Z, Yao Y et al (2018) Predictive value of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio for acute deep vein thrombosis after total joint arthroplasty: a retrospective study. J Orthop Surg Res 13:40. https://doi.org/10.1186/s13018-018-0745-x
Chen G, Wu C, Luo Z et al (2016) Platelet-lymphocyte ratios: a potential marker for pulmonary tuberculosis diagnosis in COPD patients. Int J Chron Obstruct Pulmon Dis 11:2737–2740. https://doi.org/10.2147/COPD.S111254
Gölge UH, Kaymaz B, Pazarcı Ö et al (2016) Nötrofil Lenfosit Orani Protezli Eklem Enfeksiyonlarinda Tanısal Belirteç Olabilir. J Clin Anal Med 7:218–221. https://doi.org/10.4328/JCAM.3918
Sigmund IK, Holinka J, Staats K et al (2021) Inferior performance of established and novel serum inflammatory markers in diagnosing periprosthetic joint infections. Int Orthop 45:837–846. https://doi.org/10.1007/s00264-020-04889-z
Zhang Z, Ji Y, Wang Z et al (2018) The association between platelet indices and deep surgical site infection after open induction internal fixation for traumatic limb fractures. Infect Drug Resist 11:2533–2538. https://doi.org/10.2147/IDR.S184877
Li S, Liu K, Zhang R et al (2019) Lower lymphocyte to monocyte ratio is a potential predictor of poor outcome in patients with cerebral venous sinus thrombosis. Stroke Vasc Neurol 4:148–153. https://doi.org/10.1136/svn-2018-000180
Lin Y, Peng Y, Chen Y et al (2019) Association of lymphocyte to monocyte ratio and risk of in-hospital mortality in patients with acute type A aortic dissection. Biomark Med 13:1263–1272. https://doi.org/10.2217/bmm-2018-0423
Eo WK, Chang HJ, Kwon SH et al (2016) The lymphocyte-monocyte ratio predicts patient survival and aggressiveness of ovarian cancer. J Cancer 7:289–296. https://doi.org/10.7150/jca.13432
Inaoka K, Kanda M, Uda H et al (2017) Clinical utility of the platelet-lymphocyte ratio as a predictor of postoperative complications after radical gastrectomy for clinical T2–4 gastric cancer. World J Gastroenterol 23:2519–2526. https://doi.org/10.3748/wjg.v23.i14.2519
Xu H, Xie J-W, Liu L, et al (2021) Combination of CRP with NLR is a sensitive tool for screening fixation-related infection in patients undergoing conversion total hip arthroplasty after failed internal fixation for femoral neck fracture. Bone Joint J 103-B:1534–1540. https://doi.org/10.1302/0301-620X.103B.BJJ-2021-0105.R1
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained for the retrospective patient chart review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Klemt, C., Tirumala, V., Smith, E.J. et al. Complete blood platelet and lymphocyte ratios increase diagnostic accuracy of periprosthetic joint infection following total hip arthroplasty. Arch Orthop Trauma Surg 143, 1441–1449 (2023). https://doi.org/10.1007/s00402-021-04309-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04309-w