Abstract
Introduction
Ligament bracing augments ligament repair using a non-absorbable suture tape. Although biomechanically an increase in primary stability has been proven, there is a lack of clinical evidence. Purpose of this study was to evaluate clinical results of patients treated with ligament bracing due to primary elbow instability, including an analysis of complications. Furthermore, clinical results for patients treated with and without early functional mobilization were compared.
Materials and methods
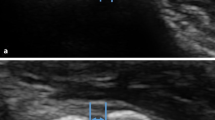
This prospective case-series evaluated clinical and functional results from patients treated with ligament bracing due to primary elbow instability. Clinical outcome measures were range of motion (ROM) as well as objective and subjective elbow scores [Mayo Elbow Performance Score (MEPS); Disabilities of Arm, Shoulder and Hand Score (DASH score)]. Stability was evaluated sonographically by humero-radial gapping under varus stress.
Results
This study involved 34 patients treated with ligament bracing. After a mean follow-up of 12.9 months ROM was 112° ± 29, MEPS 88 ± 13 points, DASH 91 ± 11 points, and 84% were satisfied with their result. Lateral joint gapping was 2.4 mm. No significant difference was observed regarding a postoperative mobilization with and without limitations. Most common complication after ligament bracing was elbow stiffness including heterotopic ossifications in four patients (12%).
Conclusion
Operatively treated elbow instability with additional ligament bracing results in good clinical outcomes with high patient satisfaction and recovery of elbow stability. The high primary stability of the ligament bracing allows early functional mobilization without bracing, which facilitates postoperative rehabilitation. Elbow stiffness with heterotopic ossification seems to be a potential complication. Furthermore, the optimal tensioning of the ligament bracing remains challenging, including the risk of an over tensioning.
Level of evidence
III.



Similar content being viewed by others
References
Stoneback JW, Owens BD, Sykes J et al (2012) Incidence of elbow dislocations in the United States population. J Bone Joint Surg Am 94:240–245
Josefsson PO, Nilsson BE (1986) Incidence of elbow dislocation. Acta Orthop Scand 57:537–538. https://doi.org/10.3109/17453678609014788
O’Driscoll S, Morrey B, Korinek S, An K (1992) Elbow subluxation and dislocation—a spectrum of instability. Clin Orthop Relat Res 186–97
O’Driscoll SW, Jupiter JB, King GJ et al (2001) The unstable elbow. Instr Course Lect 50:89–102
Kim BS, Park KH, Song HS, Park SY (2013) Ligamentous repair of acute lateral collateral ligament rupture of the elbow. J Shoulder Elbow Surg 22:1469–1473. https://doi.org/10.1016/j.jse.2013.06.018
Dehlinger F, Franke S, Hollinger B (2012) Therapeutic options for acute and chronic elbow instability. Eur J Trauma Emerg Surg 38:585–592. https://doi.org/10.1007/s00068-012-0205-y
Duckworth AD, Ring D, Kulijdian A, McKee MD (2008) Unstable elbow dislocations. J Shoulder Elbow Surg 17:281–286. https://doi.org/10.1016/j.jse.2007.06.007
Pennig D, Gausepohl T, Mader K (2000) Transarticular fixation with the capacity for motion in fracture dislocations of the elbow. Injury 31(Suppl 1):35–44
Frank J, Howorka A, Marzi I (2011) Treatment of complex elbow injuries with the hinged fixation device DJD II. Technique and results. Orthopäde 40:316–322. https://doi.org/10.1007/s00132-010-1669-2
Hopf JC, Berger V, Krieglstein CF et al (2015) Treatment of unstable elbow dislocations with hinged elbow fixation-subjective and objective results. J Shoulder Elbow Surg 24:250–257. https://doi.org/10.1016/j.jse.2014.09.034
Bhide PP, Greiner S (2018) Ligament bracing of the elbow. Obere Extrem 13:218–220. https://doi.org/10.1007/s11678-018-0463-3
Scheiderer B, Imhoff FB, Kia C et al (2020) LUCL internal bracing restores posterolateral rotatory stability of the elbow. Knee Surg Sports Traumatol Arthrosc 28:1195–1201. https://doi.org/10.1007/s00167-019-05632-x
Ellwein A, Füßler L, Ferle M et al (2021) Suture tape augmentation of the lateral ulnar collateral ligament increases load to failure in simulated posterolateral rotatory instability. Knee Surg Sports Traumatol Arthrosc 29:284–291. https://doi.org/10.1007/s00167-020-05918-5
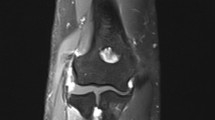
Hackl M, Wegmann K, Ries C et al (2015) Reliability of magnetic resonance imaging signs of posterolateral rotatory instability of the elbow. J Hand Surg Am 40:1428–1433. https://doi.org/10.1016/j.jhsa.2015.04.029
O’Driscoll SW (2000) Classification and evaluation of recurrent instability of the elbow. Clin Orthop Relat Res 370:34–43. https://doi.org/10.1097/00003086-200001000-00005
Camp CL, O’Driscoll SW, Wempe MK, Smith J (2017) The Sonographic Posterolateral Rotatory Stress Test for Elbow Instability: A Cadaveric Validation Study. PM R 9:275–282. https://doi.org/10.1016/j.pmrj.2016.06.014
Lee AT, Schrumpf MA, Choi D et al (2013) The influence of gravity on the unstable elbow. J Shoulder Elbow Surg 22:81–87. https://doi.org/10.1016/j.jse.2012.08.012
Mason ML (1954) Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg 42:123–132. https://doi.org/10.1002/bjs.18004217203
O’Driscoll SW, Jupiter JB, Cohen MS et al (2003) Difficult elbow fractures: pearls and pitfalls. Instr Course Lect 52:113–134
Greiner S, Koch M, Kerschbaum M, Bhide PP (2019) Repair and augmentation of the lateral collateral ligament complex using internal bracing in dislocations and fracture dislocations of the elbow restores stability and allows early rehabilitation. Knee Surg Sports Traumatol Arthrosc 27:3269–3275. https://doi.org/10.1007/s00167-019-05402-9
Heo YM, Yi JW, Lee JB et al (2015) Unstable simple elbow dislocation treated with the repair of lateral collateral ligament complex. Clin Orthop Surg 7:241–247. https://doi.org/10.4055/cios.2015.7.2.241
Daluiski A, Schrumpf MA, Schreiber JJ et al (2014) Direct repair for managing acute and chronic lateral ulnar collateral ligament disruptions. J Hand Surg Am 39:1125–1129. https://doi.org/10.1016/j.jhsa.2014.02.011
Sanchez-Sotelo J, Morrey BF, O’Driscoll SW (2018) Ligamentous repair and reconstruction for posterolateral rotatory instability of the elbow. J Bone Joint Surg Br 87-B:54–61. https://doi.org/10.1302/0301-620x.87b1.15096
Rodriguez MJ, Kusnezov NA, Dunn JC et al (2018) Functional outcomes following lateral ulnar collateral ligament reconstruction for symptomatic posterolateral rotatory instability of the elbow in an athletic population. J Shoulder Elbow Surg 27:112–117. https://doi.org/10.1016/j.jse.2017.08.015
Jung HS, Lee JS, Rhyou IH et al (2019) Dual reconstruction of lateral collateral ligament is safe and effective in treating posterolateral rotatory instability of the elbow. Knee Surg Sports Traumatol Arthrosc 27:3284–3290. https://doi.org/10.1007/s00167-019-05525-z
Reuter S, Proier P, Imhoff A, Lenich A (2016) Rehabilitation, clinical outcome and return to sporting activities after posterolateral elbow instability—a systematic review. Eur J Phys Rehabil Med 57:265–272. https://doi.org/10.23736/S1973-9087.16.04008-X
Hackl M, Leschinger T, Müller LP, Wegmann K (2019) Evidence-based treatment of ligamentous elbow dislocation. Obere Extrem 14:27–32. https://doi.org/10.1007/s11678-018-0493-x
Ring D, Bruinsma WE, Jupiter JB (2014) Complications of hinged external fixation compared with cross-pinning of the elbow for acute and subacute instability. Clin Orthop Relat Res 472:2044–2048. https://doi.org/10.1007/s11999-014-3510-4
Cheung EV, O’Driscoll SW, Morrey BF (2008) Complications of hinged external fixators of the elbow. J Shoulder Elbow Surg 17:447–453. https://doi.org/10.1016/j.jse.2007.10.006
Goren D, Budoff JE, Hipp JA (2010) Isometric placement of lateral ulnar collateral ligament reconstructions: a biomechanical study. Am J Sports Med 38:153–159. https://doi.org/10.1177/0363546509346049
Funding
No funding was received for conduction this study.
Author information
Authors and Affiliations
Contributions
All authors have substantial contribution to this study. All authors have reviewed and confirmed the accuracy of the whole manuscript before submission.
Corresponding author
Ethics declarations
Conflict of interest
Helmut Lill is consultant for Arthrex. Alexander Ellwein received speakers’ honorarium from Arthrex. All other authors declare that they have no conflict of interest.
Ethics approval
All work complied with the principles laid down in the 1964 Declaration of Helsinki and its later amendments. The study was approved by the local ethics committee (No. 7583). The study was registered at the German register for clinical studies (DRKS00012813).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ellwein, A., Janning, L., DeyHazra, RO. et al. Prospective clinical results of an additive ligament bracing for stabilizing simple and complex elbow instabilities. Arch Orthop Trauma Surg 142, 3837–3844 (2022). https://doi.org/10.1007/s00402-021-04276-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04276-2