Abstract
Purpose
To assess the clinical outcome and survival of an inlay resurfacing prosthesis for focal femoral condyle chondral and osteochondral defects.
Methods
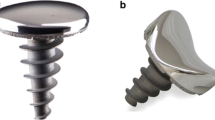
Two hundred sixty-six patients (mean age, 38.25 years; range 25–56 years) with symptomatic femoral condyle chondral and osteochondral defects were reviewed. The mean follow-up period was 7.3 years (range 5–10 years). The medial femoral condyle was involved in 229 and the lateral condyle in 37 patients. Previous cartilage surgery was done in 235 patients. All patients were treated with focal femoral condyle resurfacing with the HemiCAP® device. The preoperative and the last follow-up values of the Knee Injury and Osteoarthritis Outcome Score (KOOS), Oxford Knee Score (OKS), 36-item Short Form Survey (SF-36) and Visual Analogue Scale (VAS) were examined. Complications, reoperation rate and survival were analyzed.
Results
At the last follow-up, all clinical score values showed significant improvement as compared with the corresponding preoperative values (p < 0.001). Age presented a negative correlation with KOOS (p = 0.03) and SF-36 improvement (p = 0.014). Kellgren-Lawrence grade influenced OKS (p = 0.036). BMI, gender, side, medial or lateral condyle and size did not affect the outcome. Patients who had previous biological cartilage procedures demonstrated better clinical improvement in comparison with those that did not have prior surgery (p < 0.05). Survival was 96.2% at 10 years, using as endpoint implant revision or/and progression of osteoarthritis. The cumulative hazard for any-reason reoperation was 12.0%.
Conclusions
Femoral condyle resurfacing using the HemiCAP® device is an effective treatment option to address focal chondral and osteochondral defects. It can be successfully used either as a primary procedure or after prior biological cartilage reconstruction. Subjective clinical outcomes are expected to be good to excellent in mid- to long term, while reoperation and revision rates are low. Progression of osteoarthritis is the most common mode of failure; thus, patient selection is very important.
Level of evidence
Level IV, retrospective case series.


Similar content being viewed by others
References
Davies-Tuck ML, Wluka AE, Wang Y, Teichtahl AJ, Jones G, Ding C, Cicuttini FM (2008) The natural history of cartilage defects in people with knee osteoarthritis. Osteoarthr Cartil 16(3):337–342. https://doi.org/10.1016/j.joca.2007.07.005
de Windt TS, Bekkers JE, Creemers LB, Dhert WJ, Saris DB (2009) Patient profiling in cartilage regeneration: prognostic factors determining success of treatment for cartilage defects. Am J Sports Med 37(Suppl 1):58S-62S. https://doi.org/10.1177/0363546509349765
Goyal D, Keyhani S, Goyal A, Lee EH, Hui JH, Vaziri AS (2014) Evidence-based status of osteochondral cylinder transfer techniques: a systematic review of level I and II studies. Arthroscopy 30(4):497–505. https://doi.org/10.1016/j.arthro.2013.12.023
Peterson L, Minas T, Brittberg M, Lindahl A (2003) Treatment of osteochondritis dissecans of the knee with autologous chondrocyte transplantation: results at two to ten years. J Bone Jt Surg Am 85(2):17–24. https://doi.org/10.2106/00004623-200300002-00003
Steadman JR, Rodkey WG, Rodrigo JJ (2001) Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res 391:S362–S369. https://doi.org/10.1097/00003086-200110001-00033
Vanlauwe J, Saris DB, Victor J, Almqvist KF, Bellemans J, Luyten FP, Tig/Act, Group EXTS (2011) Five-year outcome of characterized chondrocyte implantation versus microfracture for symptomatic cartilage defects of the knee: early treatment matters. Am J Sports Med 39(12):2566–2574. https://doi.org/10.1177/0363546511422220
Knutsen G, Drogset JO, Engebretsen L, Grontvedt T, Isaksen V, Ludvigsen TC, Roberts S, Solheim E, Strand T, Johansen O (2007) A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Jt Surg Am 89(10):2105–2112. https://doi.org/10.2106/JBJS.G.00003
Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG (2003) Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy 19(5):477–484. https://doi.org/10.1053/jars.2003.50112
Furnes O, Espehaug B, Lie SA, Vollset SE, Engesaeter LB, Havelin LI (2007) Failure mechanisms after unicompartmental and tricompartmental primary knee replacement with cement. J Bone Jt Surg Am Vol 89(3):519–525. https://doi.org/10.2106/JBJS.F.00210
Gioe TJ, Novak C, Sinner P, Ma W, Mehle S (2007) Knee arthroplasty in the young patient: survival in a community registry. Clin Orthop Relat Res 464:83–87. https://doi.org/10.1097/BLO.0b013e31812f79a9
Harrysson OL, Robertsson O, Nayfeh JF (2004) Higher cumulative revision rate of knee arthroplasties in younger patients with osteoarthritis. Clin Orthop Relat Res 421:162–168. https://doi.org/10.1097/01.blo.0000127115.05754.ce
Julin J, Jamsen E, Puolakka T, Konttinen YT, Moilanen T (2010) Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis. A follow-up study of 32,019 total knee replacements in the Finnish arthroplasty register. Acta Orthop 81(4):413–419. https://doi.org/10.3109/17453674.2010.501747
Fuchs A, Eberbach H, Izadpanah K, Bode G, Sudkamp NP, Feucht MJ (2018) Focal metallic inlay resurfacing prosthesis for the treatment of localized cartilage defects of the femoral condyles: a systematic review of clinical studies. Knee Surg Sports Traumatol Arthrosc 26(9):2722–2732. https://doi.org/10.1007/s00167-017-4714-4
Brennan SA, Devitt BM, O’Neill CJ, Nicholson P (2013) Focal femoral condyle resurfacing. Bone Jt J 95-B(3):301–304. https://doi.org/10.1302/0301-620X.95B3.29998
Becher C, Huber R, Thermann H, Ezechieli L, Ostermeier S, Wellmann M, von Skrbensky G (2011) Effects of a surface matching articular resurfacing device on tibiofemoral contact pressure: results from continuous dynamic flexion-extension cycles. Arch Orthop Trauma Surg 131(3):413–419. https://doi.org/10.1007/s00402-010-1201-5
Roos EM, Toksvig-Larsen S (2003) Knee injury and osteoarthritis outcome score (KOOS)-validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 1:17. https://doi.org/10.1186/1477-7525-1-17
Bekkers JE, de Windt TS, Raijmakers NJ, Dhert WJ, Saris DB (2009) Validation of the knee injury and osteoarthritis outcome score (KOOS) for the treatment of focal cartilage lesions. Osteoarthr Cartil 17(11):1434–1439. https://doi.org/10.1016/j.joca.2009.04.019
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Jt Surg Br 80(1):63–69. https://doi.org/10.1302/0301-620x.80b1.7859
Hawker G, Melfi C, Paul J, Green R, Bombardier C (1995) Comparison of a generic (SF-36) and a disease specific (WOMAC) (Western Ontario and McMaster Universities Osteoarthritis Index) instrument in the measurement of outcomes after knee replacement surgery. J Rheumatol 22(6):1193–1196
Bijur PE, Silver W, Gallagher EJ (2001) Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med 8(12):1153–1157. https://doi.org/10.1111/j.1553-2712.2001.tb01132.x
Becher C, Huber R, Thermann H, Paessler HH, Skrbensky G (2008) Effects of a contoured articular prosthetic device on tibiofemoral peak contact pressure: a biomechanical study. Knee Surg Sports Traumatol Arthrosc 16(1):56–63. https://doi.org/10.1007/s00167-007-0416-7
Martinez-Carranza N, Hultenby K, Lagerstedt AS, Schupbach P, Berg HE (2019) Cartilage health in knees treated with metal resurfacing implants or untreated focal cartilage lesions: a preclinical study in sheep. Cartilage 10(1):120–128. https://doi.org/10.1177/1947603517720260
Kirker-Head CA, Van Sickle DC, Ek SW, McCool JC (2006) Safety of, and biological and functional response to, a novel metallic implant for the management of focal full-thickness cartilage defects: preliminary assessment in an animal model out to 1 year. J Orthop Res: Off Publ Orthop Res Soc 24(5):1095–1108. https://doi.org/10.1002/jor.20120
Beyzadeoglu T, Pehlivanoglu T (2018) Biological response following inlay arthroplasty of the knee: cartilage flow over the implant. Cartilage 9(2):156–160. https://doi.org/10.1177/1947603517746723
Dhollander AAM, Almqvist KF, Moens K, Vandekerckhove PJ, Verdonk R, Verdonk P, Victor J (2015) The use of a prosthetic inlay resurfacing as a salvage procedure for a failed cartilage repair. Knee Surg Sports Traumatol Arthrosc 23(8):2208–2212. https://doi.org/10.1007/s00167-014-2999-0
Laursen JO, Lind M (2017) Treatment of full-thickness femoral cartilage lesions using condyle resurfacing prosthesis. Knee Surg Sports Traumatol Arthrosc 25(3):746–751. https://doi.org/10.1007/s00167-015-3726-1
Stalman A, Skoldenberg O, Martinez-Carranza N, Roberts D, Hogstrom M, Ryd L (2018) No implant migration and good subjective outcome of a novel customized femoral resurfacing metal implant for focal chondral lesions. Knee Surg Sports Traumatol Arthrosc 26(7):2196–2204. https://doi.org/10.1007/s00167-017-4805-2
Laursen JO, Backer Mogensen C, Skjot-Arkil H (2019) HemiCAP knee implants: mid- to long-term results. Cartilage. https://doi.org/10.1177/1947603519894732
Becher C, Kalbe C, Thermann H, Paessler HH, Laprell H, Kaiser T, Fechner A, Bartsch S, Windhagen H, Ostermeier S (2011) Minimum 5-year results of focal articular prosthetic resurfacing for the treatment of full-thickness articular cartilage defects in the knee. Arch Orthop Trauma Surg 131(8):1135–1143. https://doi.org/10.1007/s00402-011-1323-4
Becher C, Cantiller EB (2017) Focal articular prosthetic resurfacing for the treatment of full-thickness articular cartilage defects in the knee: 12-year follow-up of two cases and review of the literature. Arch Orthop Trauma Surg 137(9):1307–1317. https://doi.org/10.1007/s00402-017-2717-8
Cases E, Natera L, Anton C, Consigliere P, Guillen J, Cruz E, Garrucho M (2021) Focal inlay resurfacing for full-thickness chondral defects of the femoral medial condyle may delay the progression to varus deformity. Eur J Orthop Surg Traumatol 31(1):57–63. https://doi.org/10.1007/s00590-020-02746-8
Becher C, Huber R, Thermann H, Tibesku CO, von Skrbensky G (2009) Tibiofemoral contact mechanics with a femoral resurfacing prosthesis and a non-functional meniscus. Clin Biomech (Bristol, Avon) 24(8):648–654. https://doi.org/10.1016/j.clinbiomech.2009.05.013
Bollars P, Bosquet M, Vandekerckhove B, Hardeman F, Bellemans J (2012) Prosthetic inlay resurfacing for the treatment of focal, full thickness cartilage defects of the femoral condyle: a bridge between biologics and conventional arthroplasty. Knee Surg Sports Traumatol Arthrosc 20(9):1753–1759. https://doi.org/10.1007/s00167-011-1757-9
van Buul GM, Stanclik J, van der Stok J, Queally JM, O’Donnell T (2021) Focal articular surface replacement of knee lesions after failed cartilage repair using focal metallic implants: a series of 132 cases with 4-year follow-up. Knee 29:134–141. https://doi.org/10.1016/j.knee.2021.01.014
Mithoefer K, Williams RJ 3rd, Warren RF, Wickiewicz TL, Marx RG (2006) High-impact athletics after knee articular cartilage repair: a prospective evaluation of the microfracture technique. Am J Sports Med 34(9):1413–1418. https://doi.org/10.1177/0363546506288240
Gill TJ (2000) The treatment of articular cartilage defects using microfracture and debridement. Am J Knee Surg 13(1):33–40
Minas T, Gomoll AH, Rosenberger R, Royce RO, Bryant T (2009) Increased failure rate of autologous chondrocyte implantation after previous treatment with marrow stimulation techniques. Am J Sports Med 37(5):902–908. https://doi.org/10.1177/0363546508330137
Oussedik S, Tsitskaris K, Parker D (2015) Treatment of articular cartilage lesions of the knee by microfracture or autologous chondrocyte implantation: a systematic review. Arthroscopy 31(4):732–744. https://doi.org/10.1016/j.arthro.2014.11.023
Pascual-Garrido C, Daley E, Verma NN, Cole BJ (2017) A comparison of the outcomes for cartilage defects of the knee treated with biologic resurfacing versus focal metallic implants. Arthroscopy 33(2):364–373. https://doi.org/10.1016/j.arthro.2016.07.010
Chahal J, Thiel GV, Hussey K, Cole BJ (2013) Managing the patient with failed cartilage restoration. Sports Med Arthrosc Rev 21(2):62–68. https://doi.org/10.1097/JSA.0b013e3182900608
Cepni S, Veizi E, Tahta M, Uluyardimci E, Abughalwa MJT, Isik C (2020) Focal metallic inlay resurfacing prosthesis in articular cartilage defects: short-term results of 118 patients and 2 different implants. Arch Orthop Trauma Surg 140(2):209–218. https://doi.org/10.1007/s00402-019-03305-5
Bedi A, Feeley BT, Williams RJ 3rd (2010) Management of articular cartilage defects of the knee. J Bone Jt Surg Am Vol 92(4):994–1009. https://doi.org/10.2106/JBJS.I.00895
Biant LC, Bentley G, Vijayan S, Skinner JA, Carrington RW (2014) Long-term results of autologous chondrocyte implantation in the knee for chronic chondral and osteochondral defects. Am J Sports Med 42(9):2178–2183. https://doi.org/10.1177/0363546514539345
Horton MT, Pulido PA, McCauley JC, Bugbee WD (2013) Revision osteochondral allograft transplantations: do they work? Am J Sports Med 41(11):2507–2511. https://doi.org/10.1177/0363546513500628
Danish OA (2015) National joint replacement registry (DKR) annual report
Australian OA (2016) National joint replacement registry. Annual report 2016
Jeschke E, Citak M, Gunster C, Matthias Halder A, Heller KD, Malzahn J, Niethard FU, Schrader P, Zacher J, Gehrke T (2017) Are TKAs performed in high-volume hospitals less likely to undergo revision than TKAs performed in low-volume hospitals? Clin Orthop Relat Res 475(11):2669–2674. https://doi.org/10.1007/s11999-017-5463-x
Laursen JO, Lind M, Mogensen CB, Skjot-Arkil H (2020) A longterm prospective follow-up study of resurfacing miniprosthesis suitable for patients above sixtyfive years with localized cartilage lesions or early osteoarthritis in the knee. J Exp Orthop 7(1):96. https://doi.org/10.1186/s40634-020-00308-9
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Megaloikonomos, P.D., Becher, C., Van der Stok, J. et al. Femoral condyle resurfacing using an inlay metal implant: low revision rate of 266 patients in a 5–10 years follow-up. Arch Orthop Trauma Surg 143, 1243–1251 (2023). https://doi.org/10.1007/s00402-021-04251-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04251-x