Abstract
Introduction
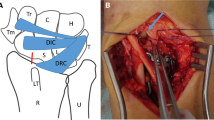
Distal radius fractures (DRFs) are very common. One of the most significant complications after intraarticular DRF is arthrofibrosis with loss of wrist motion and pain. Wrist arthroscopy has become increasingly popular in the treatment of DRF with the advantage of good visualization of the joint surface and soft tissue injuries. In intraarticular DRFs injuries of the dorsal capsule are a characteristic finding which potentially cause loss of wrist motion. In this study, we investigated if arthroscopic debridement of dorsal capsule injuries at time of surgical fixation provides superior outcomes compared to the same treatment without debridement.
Materials and methods
Between 2013 and 2017, we included 42 patients who underwent arthroscopy-assisted palmar plating for intraarticular DRFs in a prospective randomized controlled study. In group A (intervention group), the dorsal capsule tears were debrided during primary surgery, while in group B these were left in place. Active range of motion (AROM), grip strength, subjective outcomes and radiographic results were assessed 3, 6 and 12 months after primary surgery. A subgroup analysis was performed for patient age, fracture severity and duration of immobilization.
Results
Arthroscopic debridement of the dorsal capsule improved AROM in patients over 60 years of age, more severe fractures (AO 23 C2/C3) and prolonged postoperative immobilization for more than two weeks, while it was not relevant for younger patients with simple fractures and short immobilization.
Conclusions
Debridement of the injured dorsal capsule in arthroscopic-assisted surgical treatment of intraarticular DRFs can improve surgical performance and optimize patient outcomes in a specific subgroup of patients.




Similar content being viewed by others
References
Smeraglia F, Del Buono A, Maffulli N (2016) Wrist arthroscopy in the management of articular distal radius fractures. Br Med Bull 119(1):157–165. https://doi.org/10.1093/bmb/ldw032
Bentohami A, Bosma J, Akkersdijk GJ, van Dijkman B, Goslings JC, Schep NW (2014) Incidence and characteristics of distal radial fractures in an urban population in The Netherlands. Eur J Trauma Emerg Surg 40(3):357–361. https://doi.org/10.1007/s00068-014-0394-7
Pechlaner S, Gabl M, Lutz M, Krappinger D, Leixnering M, Krulis B, Ulmer H, Rudisch A, Arbeitsgruppe A (2007) Distal radius fractures–aetiology, treatment and outcome. Handchir Mikrochir Plast Chir 39(1):19–28. https://doi.org/10.1055/s-2007-964920
Knirk JL, Jupiter JB (1986) Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am 68(5):647–659
Fernandez DL, Geissler WB (1991) Treatment of displaced articular fractures of the radius. J Hand Surg Am 16(3):375–384. https://doi.org/10.1016/0363-5023(91)90001-r
Geissler WB, Freeland AE, Savoie FH, McIntyre LW, Whipple TL (1996) Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Jt Surg Am 78(3):357–365. https://doi.org/10.2106/00004623-199603000-00006
Swart E, Tang P (2017) The effect of ligament injuries on outcomes of operatively treated distal radius fractures. Am J Orthop (Belle Mead NJ) 46(1):E41–E46
Gabl M, Arora R, Klauser AS, Schmidle G (2016) Characteristics of secondary arthrofibrosis after intra-articular distal radius fracture. Arch Orthop Trauma Surg 136(8):1181–1188. https://doi.org/10.1007/s00402-016-2490-0
Anderson DD, Bell AL, Gaffney MB, Imbriglia JE (1996) Contact stress distributions in malreduced intraarticular distal radius fractures. J Orthop Trauma 10(5):331–337. https://doi.org/10.1097/00005131-199607000-00007
Geissler WB, Fernandez DL (1991) Percutaneous and limited open reduction of the articular surface of the distal radius. J Orthop Trauma 5(3):255–264. https://doi.org/10.1097/00005131-199109000-00002
Trumble TE, Schmitt SR, Vedder NB (1994) Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg Am 19(2):325–340. https://doi.org/10.1016/0363-5023(94)90028-0
Trumble TE, Wagner W, Hanel DP, Vedder NB, Gilbert M (1998) Intrafocal (Kapandji) pinning of distal radius fractures with and without external fixation. J Hand Surg Am 23(3):381–394. https://doi.org/10.1016/S0363-5023(05)80455-1
Ono H, Katayama T, Furuta K, Suzuki D, Fujitani R, Akahane M (2012) Distal radial fracture arthroscopic intraarticular gap and step-off measurement after open reduction and internal fixation with a volar locked plate. J Orthop Sci 17(4):443–449. https://doi.org/10.1007/s00776-012-0226-8
Catalano LW 3rd, Cole RJ, Gelberman RH, Evanoff BA, Gilula LA, Borrelli J Jr (1997) Displaced intra-articular fractures of the distal aspect of the radius. Long-term results in young adults after open reduction and internal fixation. J Bone Jt Surg Am 79(9):1290–1302. https://doi.org/10.2106/00004623-199709000-00003
Goldfarb CA, Rudzki JR, Catalano LW, Hughes M, Borrelli J Jr (2006) Fifteen-year outcome of displaced intra-articular fractures of the distal radius. J Hand Surg Am 31(4):633–639. https://doi.org/10.1016/j.jhsa.2006.01.008
Geissler WB, Freeland AE (1999) Arthroscopic management of intra-articular distal radius fractures. Hand Clin 15(3):455–465 (viii)
Lutsky K, Boyer MI, Steffen JA, Goldfarb CA (2008) Arthroscopic assessment of intra-articular distal radius fractures after open reduction and internal fixation from a volar approach. J Hand Surg Am 33(4):476–484. https://doi.org/10.1016/j.jhsa.2007.12.009
Edwards CC 2nd, Haraszti CJ, McGillivary GR, Gutow AP (2001) Intra-articular distal radius fractures: arthroscopic assessment of radiographically assisted reduction. J Hand Surg Am 26(6):1036–1041. https://doi.org/10.1053/jhsu.2001.28760
Abe Y, Yoshida K, Tominaga Y (2013) Less invasive surgery with wrist arthroscopy for distal radius fracture. J Orthop Sci 18(3):398–404. https://doi.org/10.1007/s00776-013-0371-8
Auge WK 2nd, Velazquez PA (2000) The application of indirect reduction techniques in the distal radius: the role of adjuvant arthroscopy. Arthroscopy 16(8):830–835. https://doi.org/10.1053/jars.2000.17717
Geissler WB (2005) Intra-articular distal radius fractures: the role of arthroscopy? Hand Clin 21(3):407–416. https://doi.org/10.1016/j.hcl.2005.02.009
Varitimidis SE, Basdekis GK, Dailiana ZH, Hantes ME, Bargiotas K, Malizos K (2008) Treatment of intra-articular fractures of the distal radius: fluoroscopic or arthroscopic reduction? J Bone Jt Surg Br 90(6):778–785. https://doi.org/10.1302/0301-620X.90B6.19809
Ruch DS, Vallee J, Poehling GG, Smith BP, Kuzma GR (2004) Arthroscopic reduction versus fluoroscopic reduction in the management of intra-articular distal radius fractures. Arthroscopy 20(3):225–230. https://doi.org/10.1016/j.arthro.2004.01.010
Doi K, Hattori Y, Otsuka K, Abe Y, Yamamoto H (1999) Intra-articular fractures of the distal aspect of the radius: arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Jt Surg Am 81(8):1093–1110. https://doi.org/10.2106/00004623-199908000-00005
Yamazaki H, Uchiyama S, Komatsu M, Hashimoto S, Kobayashi Y, Sakurai T, Kato H (2015) Arthroscopic assistance does not improve the functional or radiographic outcome of unstable intra-articular distal radial fractures treated with a volar locking plate: a randomised controlled trial. Bone Jt J 97-B(7):957–962. https://doi.org/10.1302/0301-620X.97B7.35354
Leclercq C, Mathoulin C, Members of E (2016) Complications of wrist arthroscopy: a multicenter study based on 10,107 arthroscopies. J Wrist Surg 5(4):320–326. https://doi.org/10.1055/s-0036-1584163
Lindau T (2017) Arthroscopic evaluation of associated soft tissue injuries in distal radius fractures. Hand Clin 33(4):651–658. https://doi.org/10.1016/j.hcl.2017.07.015
Adolfsson L, Jorgsholm P (1998) Arthroscopically-assisted reduction of intra-articular fractures of the distal radius. J Hand Surg Br 23(3):391–395. https://doi.org/10.1016/s0266-7681(98)80065-x
Richards RS, Bennett JD, Roth JH, Milne K Jr (1997) Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg Am 22(5):772–776. https://doi.org/10.1016/S0363-5023(97)80068-8
Lindau T, Adlercreutz C, Aspenberg P (2000) Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J Hand Surg Am 25(3):464–468. https://doi.org/10.1053/jhsu.2000.6467
Forward DP, Lindau TR, Melsom DS (2007) Intercarpal ligament injuries associated with fractures of the distal part of the radius. J Bone Joint Surg Am 89(11):2334–2340. https://doi.org/10.2106/JBJS.F.01537
Shkolnikova J, Harvey J (2018) Wrist arthroscopy in the management of distal radius fractures. Annal Jt 3:77
Khanchandani P, Badia A (2013) Functional outcome of arthroscopic assisted fixation of distal radius fractures. Indian J Orthop 47(3):288–294. https://doi.org/10.4103/0019-5413.109872
Selles CA, Mulders MAM, Colaris JW, van Heijl M, Cleffken BI, Schep NWL (2020) Arthroscopic debridement does not enhance surgical treatment of intra-articular distal radius fractures: a randomized controlled trial. J Hand Surg Eur 45(4):327–332. https://doi.org/10.1177/1753193419866128
Bain GI, Munt J, Turner PC, Bergman J (2008) Arthroscopic dorsal capsular release in the wrist: a new technique. Tech Hand Up Extrem Surg 12(3):191–194. https://doi.org/10.1097/BTH.0b013e3181839bb4
Bosch U (2002) Arthrofibrosis. Orthopade 31(8):785–790. https://doi.org/10.1007/s00132-002-0336-7
Lee SK, Gargano F, Hausman MR (2006) Wrist arthrofibrosis. Hand Clin 22(4):529–538. https://doi.org/10.1016/j.hcl.2006.09.002 (abstract vii)
Steplewski A, Fertala J, Beredjiklian PK, Abboud JA, Wang MLY, Namdari S, Barlow J, Rivlin M, Arnold WV, Kostas J, Hou C, Fertala A (2017) Blocking collagen fibril formation in injured knees reduces flexion contracture in a rabbit model. J Orthop Res 35(5):1038–1046. https://doi.org/10.1002/jor.23369
Tang X, Teng S, Petri M, Krettek C, Liu C, Jagodzinski M (2018) The effect of anti-inflammatory and antifibrotic agents on fibroblasts obtained from arthrofibrotic tissue: an in vitro and in vivo study. Bone Jt Res 7(3):213–222. https://doi.org/10.1302/2046-3758.73.BJR-2017-0219.R2
Verhellen R, Bain GI (2000) Arthroscopic capsular release for contracture of the wrist: a new technique. Arthroscopy 16(1):106–110. https://doi.org/10.1016/s0749-8063(00)90137-3
Hattori T, Tsunoda K, Watanabe K, Nakao E, Hirata H, Nakamura R (2006) Arthroscopic mobilization for contracture of the wrist. Arthroscopy 22(8):850–854. https://doi.org/10.1016/j.arthro.2006.04.099
Luchetti R, Atzei A, Fairplay T (2007) Arthroscopic wrist arthrolysis after wrist fracture. Arthroscopy 23(3):255–260. https://doi.org/10.1016/j.arthro.2006.11.001
Zeckey C, Spath A, Kieslich S, Kammerlander C, Bocker W, Weigert M, Neuerburg C (2020) Early mobilization versus splinting after surgical management of distal radius fractures. Dtsch Arztebl Int 117(26):445–451. https://doi.org/10.3238/arztebl.2020.0445
Funding
No disclosures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Gernot Schmidle, Stefan Benedikt, Tobias Kastenberger, Peter Kaiser, Rohit Arora, and Markus Gabl declare that they have no conflict of interest.
Ethical approval
The study was approved by the local ethics committee (ethics committee of the Medical University Innsbruck, AN 20131161 323/4.2).
Informed consent
Informed consent was obtained from all study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 222501 KB)
Rights and permissions
About this article
Cite this article
Schmidle, G., Benedikt, S., Kastenberger, T. et al. Arthroscopic debridement of the dorsal capsule in intraarticular distal radius fractures: does it provide superior outcomes?. Arch Orthop Trauma Surg 142, 691–699 (2022). https://doi.org/10.1007/s00402-021-04246-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04246-8