Abstract
Background
Microbiological profile of pathogens causing periprosthetic joint infection (PJI) after primary total hip (THA) and knee (TKA) arthroplasty varies in different regions, clinics and even departments. The objective of this study was to analyze the pathogen structure in patients with PJI after primary THA and TKA and its influence on the effectiveness of the infection eradication after two-stage reimplantation.
Materials and methods
We collected the retrospective data of 364 patients—161 with PJI after primary TKA (113 treated in two stages 48 with failure after spacer implantation) and 203 patients with infected THA (127 after successful two-stage reimplantation and 76 with PJI recurrence after the first stage) within the time period from January 2012 to December 2017, treated with two-stage protocol in the single center. A comparative analysis of pathogen structure was performed between cohorts of patients with hip and knee PJI. A subanalysis was made between the subsets comprised from patients with successful two-stage treatment and the subsets with failure to treat the infection.
Results
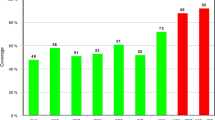
Staphylococcus epidermidis was the most commonly identified pathogen in the full hip and knee cohorts: 30.1% and 32.5%, respectively. However, the percentage of methicillin-resistant Staphylococcus epidermidis (MRSE) among all S. epidermidis isolates was higher in the hip cohort—50% compared with 35% in the knee cohort (p = 0.073). Other coagulase-negative Staphylococci were more common to patients with PJI after primary TKA—10.3% compared with 5% (p < 0.02). Streptococcus sp. caused hip PJI in a larger percentage of cases than in knee PJI (p < 0.01)—7% and 2%, respectively (p < 0.01).
Polymicrobial associations were significantly more common in hip PJI compared to knee PJI: 45.3% and 14% of cases, respectively (p < 0.001). The presence of polymicrobial infection significantly raised the risk of PJI recurrence [OR 2 (95% CI from 1.24 to 3.24)] in knee PJI patients and reduced the effectiveness of infection eradication from 73.9% to 47.8%.
Conclusion
Comparative analysis showed significant differences in the structure of PJI pathogens in the hip and knee. These findings are useful when choosing treatment strategies and empirical antibiotics regimens, in the management of patients with PJIs after primary hip and knee arthroplasty.

Similar content being viewed by others
Availability of data and material
The dataset supporting the conclusions of this article is available from the corresponding author on reasonable request.
References
Aggarwal VK, Bakhshi H, Ecker NU, Parvizi J, Gehrke T, Kendoff D (2014) Organism profile in periprosthetic joint infection: pathogens differ at two arthroplasty infection referral centers in Europe and in the United States. J Knee Surg 27(5):399–406. https://doi.org/10.1055/s-0033-1364102
Akgün D, Müller M, Perka C, Winkler T (2019) High cure rate of periprosthetic hip joint infection with multidisciplinary team approach using standardized two-stage exchange. J Orthop Surg Res 14:78. https://doi.org/10.1186/s13018-019-1122-0
Akgün D, Trampuz A, Perka C, Renz N (2017) High failure rates in treatment of streptococcal periprosthetic joint infection: results from a seven-year retrospective cohort study. Bone Joint J 99-B(5):653–659. https://doi.org/10.1302/0301-620X.99B5.BJJ-2016-0851.R1
Antony SJ, Westbrook RS, Jackson JS, Heydemann JS, Nelson JL (2015) Efficacy of single-stage revision with aggressive debridement using intra-articular antibiotics in the treatment of infected joint prosthesis. Infect Dis (Auckl) 8:17–23. https://doi.org/10.4137/IDRT.S26824
Ascione T, Pagliano P, Balato G, Mariconda M, Rotondo R, Esposito S (2017) Oral therapy, microbiological findings, and comorbidity influence the outcome of prosthetic joint infections undergoing 2-stage exchange. J Arthroplasty 32(7):2239–2243. https://doi.org/10.1016/j.arth.2017.02.057
Bjerke-Kroll BT, Christ AB, McLawhorn AS, Sculco PK, Jules-Elysée KM, Sculco TP (2014) Periprosthetic joint infections treated with two-stage revision over 14 years: an evolving microbiology profile. J Arthroplasty 29(5):877–882. https://doi.org/10.1016/j.arth.2013.09.053
Boelch SP, Jakuscheit A, Doerries S, Fraissler L, Hoberg M, Arnholdt J, Rudert M (2018) Periprosthetic infection is the major indication for TKA revision—experiences from a university referral arthroplasty center. BMC Musculoskelet Disord 19(1):395. https://doi.org/10.1186/s12891-018-2314-1
Bozhkova SA, Kasimova AR, Tikhilov RM, Polyakova EM, Rukina AN, Shabanova VV, Liventsov VN (2018) Adverse trends in the etiology of orthopedic infection: results of 6 year monitoring of the structure and resistance of leading pathogens. Traumatol Orthop of Russia 24(4):20–31. https://doi.org/10.21823/2311-2905-2018-24-4-20-31 (In Russ)
Bozhkova S, Tikhilov R, Labutin D, Denisov A, Shubnyakov I, Razorenov V, Artyukh V, Rukina A (2016) Failure of the first step of two-stage revision due to polymicrobial prosthetic joint infection of the hip. J Orthop Traumatol 17(4):369–376. https://doi.org/10.21823/2311-2905-2018-24-4-20-31
Bozic KJ, Kamath AF, Ong K, Lau E, Kurtz S, Chan V, Vail TP, Rubash H, Berry DJ (2015) Comparative epidemiology of revision arthroplasty: failed THA poses greater clinical and economic burdens than failed TKA. Clin Orthop Relat Res 473(6):2131–2138. https://doi.org/10.1007/s11999-014-4078-8
Castellani L, Daneman N, Mubareka S, Jenkinson R (2017) Factors associated with choice and success of one- versus two-stage revision arthroplasty for infected hip and knee prostheses. HSS J 13(3):224–231. https://doi.org/10.1007/s11420-017-9550-z
Chen SY, Wang JT, Chen TH, Lai MS, Chie WC, Chien KL, Hsueh PR, Wang JL, Changv SC (2010) Impact of traditional hospital strain of methicillin-resistant Staphylococcus aureus (MRSA) and community strain of MRSA on mortality in patients with community-onset S aureus bacteremia. Medicine (Baltimore) 89(5):285–294. https://doi.org/10.1097/MD.0b013e3181f1851e
Dubée V, Zeller V, Lhotellier L, Kitzis MD, Ziza JM, Mamoudy P, Desplaces N (2013) Continuous high-dose vancomycin combination therapy for methicillin-resistant staphylococcal prosthetic hip infection: a prospective cohort study. Clin Microbiol Infect 19(2):E98-105. https://doi.org/10.1111/1469-0691.12071
Gundtoft PH, Pedersen AB, Varnum C, Overgaard S (2017) Increased mortality after prosthetic joint infection in primary THA. Clin Orthop Relat Res 475(11):2623–2631. https://doi.org/10.1007/s11999-017-5289-6
Hischebeth GT, Randau TM, Ploeger MM, Friedrich MJ, Kaup E, Jacobs C, Molitor E, Hoerauf A, Gravius S, Wimmer MD (2019) Staphylococcus aureus versus Staphylococcus epidermidis in periprosthetic joint infection—outcome analysis of methicillin-resistant versus methicillin-susceptible strains. Diagn Microbiol Infect Dis 93(2):125–130. https://doi.org/10.1016/j.diagmicrobio.2018.08.012
Ip D, Yam SK, Chen CK (2005) Implications of the changing pattern of bacterial infections following total joint replacements. J Orthop Surg (Hong Kong) 13(2):125–130. https://doi.org/10.1177/230949900501300204
Jhan SW, Lu YD, Lee MS, Lee CH, Wang JW, Kuo FC (2017) The risk factors of failed reimplantation arthroplasty for periprosthetic hip infection. BMC Musculoskelet Disord 18(1):255. https://doi.org/10.1186/s12891-017-1622-1
Kandel CE, Jenkinson R, Daneman N, Backstein D, Hansen BE, Muller MP, Katz KC, Widdifield J, Bogoch E, Ward S, Sajja A, Jeldes FG, McGeer A (2019) Predictors of treatment failure for hip and knee prosthetic joint infections in the setting of 1- and 2-stage exchange arthroplasty: a multicenter retrospective cohort. Open Forum Infect Dis 6(11):ofz452. https://doi.org/10.1093/ofid/ofz452
Kavolus JJ, Cunningham DJ, Rao SR, Wellman SS, Seyler TM (2019) Polymicrobial infections in hip arthroplasty: lower treatment success rate, increased surgery, and longer hospitalization. J Arthroplasty 34(4):710-716.e3. https://doi.org/10.1016/j.arth.2018.09.090
Lentino JR (2003) Prosthetic joint infections: bane of orthopedists, challenge for infectious disease specialists. Clin Infect Dis 36(9):1157–1161. https://doi.org/10.1086/374554
Parvizi J, Gehrke T (2014) International consensus group on periprosthetic joint infection. Definition of periprosthetic joint infection. J Arthroplasty 29(7):1331. https://doi.org/10.1016/j.arth.2014.03.009
Piper KE, Jacobson MJ, Cofield RH, Sperling JW, Sanchez-Sotelo J, Osmon DR, McDowell A, Patrick S, Steckelberg JM, Mandrekar JN, Fernandez Sampedro M, Patel R (2009) Microbiologic diagnosis of prosthetic shoulder infection by use of implant sonication. J Clin Microbiol 47(6):1878–1884. https://doi.org/10.1128/JCM.01686-08
Postler A, Lützner C, Beyer F, Tille E, Lützner J (2018) Analysis of total knee arthroplasty revision causes. BMC Musculoskelet Disord 19(1):55. https://doi.org/10.1186/s12891-018-1977-y
Rosteius T, Jansen O, Fehmer T, Baecker H, Citak M, Schildhauer TA, Geßmann J (2018) Evaluating the microbial pattern of periprosthetic joint infections of the hip and knee. J Med Microbiol 67(11):1608–1613. https://doi.org/10.1099/jmm.0.000835
Tsai JC, Sheng WH, Lo WY, Jiang CC, Chang SC (2015) Clinical characteristics, microbiology, and outcomes of prosthetic joint infection in Taiwan. J Microbiol Immunol Infect 48(2):198–204. https://doi.org/10.1016/j.jmii.2013.08.007
Tsai Y, Chang CH, Lin YC, Lee SH, Hsieh PH, Chang Y (2019) Different microbiological profiles between hip and knee prosthetic joint infections. J Orthop Surg (Hong Kong) 27(2):2309499019847768. https://doi.org/10.1177/2309499019847768
Wimmer MD, Friedrich MJ, Randau TM, Ploeger MM, Schmolders J, Strauss AA, Hischebeth GT, Pennekamp PH, Vavken P, Gravius S (2016) Polymicrobial infections reduce the cure rate in prosthetic joint infections: outcome analysis with two-stage exchange and follow-up ≥ two years. Int Orthop 40(7):1367–1373. https://doi.org/10.1007/s00264-015-2871-y
Zajonz D, Wuthe L, Rodloff AC, Prietzel T, von Salis-Soglio GF, Roth A, Heyde CE, Josten C, Ghanem M (2016) Infections of hip and knee endoprostheses. Spectrum of pathogens and the role of multiresistant bacteria. Chirurg 87(4):332–339. https://doi.org/10.1007/s00104-015-0126-5
Zimmerli W, Trampuz A, Ochsner PE (2004) Prosthetic-joint infections. N Engl J Med 351(16):1645–1654. https://doi.org/10.1056/NEJMra040181 (Review. PMID: 15483283)
Author information
Authors and Affiliations
Contributions
PP—development of the concept and study design of, collection, analysis and interpretation of the obtained data, statistical data processing, writing of the manuscript. SB—development of the concept and design of the study, writing and editing of the manuscript, interpretation the obtained data. AK—collection, analysis and interpretation of the obtained data, writing of the manuscript. RT—development of the concept and design of the study, editing of the manuscript. AK—development of the concept and design of the study, writing and editing of the manuscript. All authors read and approved the final version of the manuscript. All authors agree to be responsible for all aspects of the work to ensure proper consideration and resolution of all possible issues related to the correctness and reliability of any part of the work.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Preobrazhensky, P., Bozhkova, S., Kochish, A. et al. Comparative analysis of pathogen structure in patients with PJI after primary total hip and knee arthroplasty. Arch Orthop Trauma Surg 141, 1963–1969 (2021). https://doi.org/10.1007/s00402-021-04139-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04139-w