Abstract
Introduction
Recurrent dislocation represents the third most common cause of revision surgery after total hip arthroplasty (THA). However, there is a paucity of information on the outcome of revision total hip arthroplasty for recurrent dislocation. In this study, we investigated (1) clinical outcomes of patients that underwent revision THA for recurrent dislocation, and (2) potential risk factors associated with treatment failure in patients who underwent revision total hip arthroplasty for recurrent dislocation.
Methods
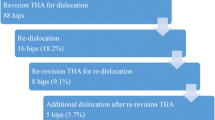
We retrospectively reviewed 211 consecutive cases of revision total hip arthroplasty for recurrent dislocation, 81 implanted with a constrained liner and 130 with a non-constrained liner with a large-diameter femoral head (> 32 mm). Patient- and implant-related risk factors were analyzed in multivariate regression analysis.
Results
At 4.6-year follow-up, 32 of 211 patients (15.1%) underwent re-revision surgery. The most common causes for re-revision included infection (14 patients) and dislocation (10 patients). Kaplan–Meier analysis demonstrates a 5-year survival probability of 77% for patients that underwent revision THA for recurrent dislocation. Osteoporosis, obesity (BMI ≥ 40), spine disease and abductor deficiency are independent risk factors for failure of revision surgery for recurrent dislocation. Liner type (constrained vs. non-constrained) was found not to be associated with failure of revision THA for recurrent dislocation (p = 0.44).
Conclusion
This study suggests that THA revision for recurrent dislocation is associated with a high re-revision rate of 15% at mid-term follow-up. Osteoporosis, obesity (BMI ≥ 40) spine disease and abductor deficiency were demonstrated to be independent risk factors for failure of revision THA for recurrent dislocation.
Level of evidence
Level III, case–control retrospective analysis.

Similar content being viewed by others
References
Khan RJK, Fick D, Alakeson R et al (2006) A constrained acetabular component for recurrent dislocation. J Bone Joint Surg Br 88:870–876. https://doi.org/10.1302/0301-620X.88B7.17644
Carlson BC, Desy NM, Johnson JD et al (2018) Modern surgical treatment of recurrent posterior dislocation of the native hip. J Bone Joint Surg Am 100:1056–1063. https://doi.org/10.2106/JBJS.17.01170
Bonner B, Arauz P, Klemt C, Kwon Y-M (2020) Outcome of re-revision surgery for adverse local tissue reaction in metal-on-polyethylene and metal-on-metal total hip arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.02.006
Malik AT, Jain N, Scharschmidt TJ et al (2018) Does surgeon volume affect outcomes following primary total hip arthroplasty? A systematic review. J Arthroplasty 33:3329–3342. https://doi.org/10.1016/j.arth.2018.05.040
Elbuluk AM, Coxe FR, Schimizzi GV et al (2020) Abductor deficiency-induced recurrent instability after total hip arthroplasty. JBJS Rev 8:e0164. https://doi.org/10.2106/JBJS.RVW.18.00164
Dammerer D, Schneider F, Renkawitz T et al (2020) High risk of hip dislocation following polyethylene liner exchange in total hip arthroplasty-is cup revision necessary? Arch Orthop Trauma Surg 140:1837–1845. https://doi.org/10.1007/s00402-020-03603-3
Hamadouche M, Biau DJ, Huten D et al (2010) The use of a cemented dual mobility socket to treat recurrent dislocation. Clin Orthop Relat Res 468:3248–3254. https://doi.org/10.1007/s11999-010-1404-7
Fricka KB, Marshall A, Paprosky WG (2006) Constrained liners in revision total hip arthroplasty: an overuse syndrome. In the affirmative. J Arthroplasty. https://doi.org/10.1016/j.arth.2006.02.100
Kaplan SJ, Thomas WH, Poss R (1987) Trochanteric advancement for recurrent dislocation after total hip arthroplasty. J Arthroplasty 2:119–124. https://doi.org/10.1016/s0883-5403(87)80018-9
Klemt C, Smith EJ, Oganesyan R et al (2020) Outcome of dual mobility constructs for adverse local tissue reaction associated abductor deficiency in revision total hip arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.06.043
Hoskins W, Griffin X, Hatton A et al (2020) THA for a fractured femoral neck: comparing the revision and dislocation rates of standard-head, large-head, dual-mobility, and constrained liners. Clin Orthop Relat Res. https://doi.org/10.1097/CORR.0000000000001447
Chalmers BP, Pallante GD, Taunton MJ et al (2018) Can dislocation of a constrained liner be salvaged with dualmobility constructs in revision THA? Clin Orthop Relat Res 476:305–312. https://doi.org/10.1007/s11999.0000000000000026
Brown TS, Tibbo ME, Arsoy D et al (2019) Long-term outcomes of constrained liners cemented into retained, well-fixed acetabular components. J Bone Jt Surg Am 101:620–627. https://doi.org/10.2106/JBJS.18.00607
Plate JF, Seyler TM, Stroh DA et al (2012) Risk of dislocation using large- vs. small-diameter femoral heads in total hip arthroplasty. BMC Res Notes 5:553. https://doi.org/10.1186/1756-0500-5-553
Lewinnek GE, Lewis JL, Tarr R et al (1978) Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 60:217–220
Karvonen M, Karvonen H, Seppänen M et al (2017) Freedom constrained liner for the treatment and prevention of dislocation in total hip arthroplasty. Scand J Surg SJS Off organ Finnish Surg Soc Scand Surg Soc 106:165–172. https://doi.org/10.1177/1457496916660035
Flecher X, Ollivier M, Argenson JN (2016) Lower limb length and offset in total hip arthroplasty. Orthop Traumatol Surg Res 102:S9-20. https://doi.org/10.1016/j.otsr.2015.11.001
Kusin DJ, Ungar JA, Samson KK, Teusink MJ (2019) Body mass index as a risk factor for dislocation of total shoulder arthroplasty in the first 30 days. JSES Open Access 3:179–182. https://doi.org/10.1016/j.jses.2019.07.001
Mendez JH, Mehrani A, Randolph P, Stagg S (2019) Throughput and resolution with a next-generation direct electron detector. IUCrJ 6:1007–1013. https://doi.org/10.1107/S2052252519012661
Kenney C, Dick S, Lea J et al (2019) A systematic review of the causes of failure of revision total hip arthroplasty. J Orthop 16:393–395. https://doi.org/10.1016/j.jor.2019.04.011
Mehta N, Selvaratnam V, Alsousou J et al (2020) Outcome of revision surgery in recurrent dislocation of primary total hip arthroplasty. Hip Int J Clin Exp Res hip Pathol Ther. https://doi.org/10.1177/1120700020911146
Herman A, Masri BA, Duncan CP et al (2020) Multivariate analysis of risk factors for re-dislocation after revision for dislocation after total hip arthroplasty. Hip Int J Clin Exp Res hip Pathol Ther 30:93–100. https://doi.org/10.1177/1120700019831628
Biviji AA, Ezzet KA, Pulido P, Colwell CWJ (2009) Modular femoral head and liner exchange for the unstable total hip arthroplasty. J Arthroplasty 24:625–630. https://doi.org/10.1016/j.arth.2008.03.015
Hernigou P, Trousselier M, Roubineau F et al (2016) Dual-mobility or constrained liners are more effective than preoperative bariatric surgery in prevention of THA dislocation. Clin Orthop Relat Res 474:2202–2210. https://doi.org/10.1007/s11999-016-4859-3
Huang C-C, Jiang C-C, Hsieh C-H et al (2016) Local bone quality affects the outcome of prosthetic total knee arthroplasty. J Orthop Res Off Publ Orthop Res Soc 34:240–248. https://doi.org/10.1002/jor.23003
Gill K, Whitehouse SL, Hubble MJW, Wilson MJ (2016) Short-term results with a constrained acetabular liner in patients at high risk of dislocation after primary total hip arthroplasty. Hip Int J Clin Exp Res hip Pathol Ther 26:580–584. https://doi.org/10.5301/hipint.5000396
Malkani AL, Himschoot KJ, Ong KL et al (2019) Does timing of primary total hip arthroplasty prior to or after lumbar spine fusion have an effect on dislocation and revision rates? J Arthroplasty 34:907–911. https://doi.org/10.1016/j.arth.2019.01.009
Esposito CI, Carroll KM, Sculco PK et al (2018) Total hip arthroplasty patients with fixed spinopelvic alignment are at higher risk of hip dislocation. J Arthroplasty 33:1449–1454. https://doi.org/10.1016/j.arth.2017.12.005
Limmahakhun S, Box HN, Arauz P et al (2019) In vivo analysis of spinopelvic kinematics and peak head-cup contact in total hip arthroplasty patients with lumbar degenerative disc disease. J Orthop Res 37:674–680. https://doi.org/10.1002/jor.24234
Klemt C, Limmahakhun S, Bounajem G et al (2020) Effect of postural changes on in vivo pelvic tilt and functional component anteversion in total hip arthroplasty patients with lumbar disc degenerations. Bone Joint J. https://doi.org/10.1302/0301-620X.102B9.BJJ-2020-0777.R1
Waterson HB, Whitehouse MR, Greidanus NV et al (2018) Revision for adverse local tissue reaction following metal-on-polyethylene total hip arthroplasty is associated with a high risk of early major complications. Bone Joint J 100-B:720–724. https://doi.org/10.1302/0301-620X.100B6.BJJ-2017-1466.R1
Gaillard R, Kenney R, Delalande J-L et al (2019) Ten- to 16-year results of a modern cementless dual-mobility acetabular implant in primary total hip arthroplasty. J Arthroplasty 34:2704–2710. https://doi.org/10.1016/j.arth.2019.06.051
Hartzler MA, Abdel MP, Sculco PK, et al (2018) Otto Aufranc award: dual-mobility constructs in revision THA reduced dislocation, rerevision, and reoperation compared with large femoral heads. In: Clinical Orthopaedics and Related Research
Abdel MP (2018) Dual-mobility constructs in revision total hip arthroplasties. J Arthroplasty 33:1328–1330. https://doi.org/10.1016/j.arth.2018.01.030
Chalmers BP, Ledford CK, Taunton MJ et al (2018) Cementation of a dual mobility construct in recurrently dislocating and high risk patients undergoing revision total arthroplasty. J Arthroplasty 33:1501–1506. https://doi.org/10.1016/j.arth.2017.11.055
Fessy M-H, Jacquot L, Rollier J-C et al (2019) Midterm clinical and radiographic outcomes of a contemporary monoblock dual-mobility cup in uncemented total hip arthroplasty. J Arthroplasty 34:2983–2991. https://doi.org/10.1016/j.arth.2019.07.026
Klemt C, Bounajem G, Tirumala V et al (2020) Three-dimensional kinematic analysis of dislocation mechanism in dual mobility total hip arthroplasty constructs. J Orthop Res Off Publ Orthop Res Soc. https://doi.org/10.1002/jor.24855
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained for the retrospective patient chart review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Klemt, C., Chen, W., Bounajem, G. et al. Outcome and risk factors of failures associated with revision total hip arthroplasty for recurrent dislocation. Arch Orthop Trauma Surg 142, 1801–1807 (2022). https://doi.org/10.1007/s00402-021-03814-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03814-2