Abstract
Background
Topical administration of tranexamic acid (TXA) in patients undergoing total knee arthroplasty (TKA) is increasingly popular as it avoids the risks related with systemic absorption of the medication. Previous studies have established the efficacy of TXA in TKA, however here are limited direct comparison studies available and the dosing regimens vary. Hence, there is no consensus on an optimal dose. Our objective is to compare blood loss, transfusion requirement and immediate post-operative function between high (2 g) and low (1 g) dose tranexamic acid in patients undergoing TKA.
Methods
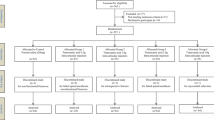
This is a retrospective cohort study of 104 patients undergoing total knee arthroplasty in a single institution under a single surgeon. In total, 61 and 43 patients receiving 1 g and 2 g of topical TXA respectively. Blood loss as estimated from the difference in haemoglobin (Hb) and haematocrit (HCT) levels post-surgery and number of blood transfusions required were compared between groups. Immediate post-operative function and complications were also measured.
Results
Patient characteristics were mostly similar between groups. The transfusion requirements were higher in 1 g group compared to the 2 g group (0.11 vs 0.00, p = 0.034). The mean post op day 1 (POD1) range of motion higher in the 1 g group vs 2 g group (72.1 vs 63.7, p = 0.035). The 2 g group had a lower POD1 pain score compared to the 1 g group (4.02 vs 5.43, p < 0.01). There was no statistically significant difference in complications that were related to the administration of TXA between the two groups.
Conclusion
Higher dose of topical TXA is safe, helps improve immediate post-operative functional outcomes and reduces transfusion requirements.
Similar content being viewed by others
References
Wu L, Li M, Zeng Y et al (2020) Prevalence and risk factors for prolonged opioid use after total joint arthroplasty: a systematic review, meta-analysis, and meta-regression. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03486-4
Dong Z, Han L, Song Y et al (2019) Hemostatic techniques to reduce blood transfusion after primary TKA: a meta-analysis and systematic review. Arch Orthop Trauma Surg 139:1785–1796
Sehat KR, Evans R, Newman JH (2000) How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee 7(3):151–155
Mi B, Liu G, Zhou W et al (2017) Intra-articular versus intravenous tranexamic acid application in total knee arthroplasty: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 137:997–1009
Wong J, Abrishami A, El Beheiry H et al (2010) Topical application of tranexamic acid reduces postoperative blood loss in total knee arthroplasty: a randomized, controlled trial. J Bone Joint Surg Am 92(15):2503–2513
Kim Y, Park J, Kim J et al (2019) Does tranexamic acid increase the risk of thromboembolism after bilateral simultaneous total knee arthroplasties in Asian population? Arch Orthop Trauma Surg 138:83–89
Panteli M, Papakostidis C, Dahabreh Z, Giannoudis PV (2013) Topical tranexamic acid in total knee replacement: a systematic review and meta-analysis. Knee 20(5):300–309
Alshryda S, Sukeik M, Sarda P, Blenkinsopp J, Haddad FS, Mason JM (2014) A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Joint J 96-b(8):1005–1015
Nattapol T, Raphi R, Supakit K (2019) High dose (3g) topical tranexamic acid has higher potency in reducing blood loss after total knee arthroplasty compared with low dose (500mg): a double-blind randomized controlled trial. Eur J Orthop Surg Traumato 29:1729–1735
Carvalho LH, Frois Temponi E, Machado Soares LF, Gonçalves MBJ, Paiva Costa L, Tavares de Souza MLA (2015) Bleeding reduction after topical application of tranexamic acid together with Betadine solution in total knee arthroplasty. A randomised controlled study. Orthopaedics Traumatol 101(1):83–87
Parvizi J, Huang R, Restrepo C et al (2017) Low-dose aspirin is effective chemoprophylaxis against clinically important venous thromboembolism following total joint arthroplasty: a preliminary analysis. J Bone Joint Surg Am 99(2):91–98. https://doi.org/10.2106/JBJS.16.00147
Kim Y, Anil V, Gaurav A et al (2019) Mechanical thromboprophylaxis would suffice after total knee arthroplasties in Asian patients? Arch Orthop Trauma Surg 139:167–171. https://doi.org/10.1007/s00402-018-3045-3
Sukeik M, Alshryda S, Haddad FS et al (2011) Systematic review and meta-analysis of the use of tranexamic acid in total hip replacement. J Bone Joint Surg Br 93:39–46
Digas G, Koutsogiannis I, Meletiadis G et al (2015) Intra-articular injection of tranexamic acid reduce blood loss in cemented total knee arthroplasty. Eur J Orthop Surg Traumatol 25:1181–1188
Sun Q, Li J, Chen J et al (2019) Comparison of intravenous, topical or combined routes of tranexamic acid administration in patients undergoing total knee and hip arthroplasty: a metaanalysis of randomised controlled trials. BMJ Open 9:e024350. https://doi.org/10.1136/bmjopen-2018-024350
Sa-Ngasoongsong P, Wongsak S, Chanplakorn P, Woratanarat P, Wechmongkolgorn S, Wibulpolprasert B, Mulpruek P, Kawinwonggowit V (2013) Efficacy of low-dose intra-articular tranexamic acid in total knee replacement; a prospective tripleblinded randomized controlled trial. BMC Musculoskelet Disord 14:340
Molloy DO, Archbold HA, Ogonda L, McConway J, Wilson RK, Beverland DE (2007) Comparison of topical fibrin spray and tranexamic acid on blood loss after total knee replacement: a prospective, randomised controlled trial. J Bone Joint Surg Br 89:306–309
Ishida K, Tsumura N, Kitagawa A, Hamamura S, Fukuda K, Dogaki Y (2011) Intra-articular injection of tranexamic acid reduces not only blood loss but also knee joint swelling after total knee arthroplasty. Int Orthop 35:1639–1645
Funding
There is no funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Ethics Committee (NHG DSRB 2019/00907).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, C., Tan, C. & Wang, L. Higher doses of topical tranexamic acid safely improves immediate functional outcomes and reduces transfusion requirement in total knee arthroplasty. Arch Orthop Trauma Surg 140, 2071–2075 (2020). https://doi.org/10.1007/s00402-020-03591-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03591-4