Abstract
Background
Digital templating is an essential step in the preoperative planning of total hip arthroplasty (THA). Previous studies have suggested that templating with the double marker method may be more accurate than a single marker method in the general population and in obese patients. The purpose of this study was to compare the accuracy in the preoperative component selection between the King Mark calibration device and the conventional metal ball method. Additionally, we examined whether King Mark offered any advantage over the standard metal ball in the preoperative selection of component sizes for obese patients.
Methods
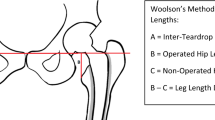
We retrospectively reviewed patients who underwent preoperative digital templating for THA in our center from January 2014 to January 2016 with King Mark device and marker ball. We compared the preoperative template component size and offset with the intraoperative definite implant size. The accuracy was defined as the difference between preoperative and intraoperative component sizes. The overall accepted calibration was defined as an exact match ± one size. Patients were stratified into two cohorts according to the calibration method: standard marker ball technique and King Mark technique.
Results
126 THA underwent digital calibration. 79 patients underwent a preoperative templating using the King Mark calibration device. 47 patients were templated using a conventional marker ball. The overall adequate preoperative planning of the acetabular cup (exact or ± 1 size match) in the King Mark group did not differ from the single marker method (74.7% and 74.5%, respectively, p = 0.979). No significant difference was noted in the overall accepted calibration of the femoral stem (exact or ± 1 size match) between the marker ball group and the King Mark group (58.2% and 70.2%, respectively, p = 0.179). The King Mark group showed a better preoperative planning for the stem’s offset compared to the marker ball group (77.2% % and 61.7%, respectively, p = 0.062). For the obese patient cohort, no significant difference was noted between the King Mark group and the marker ball group in the exact prediction of the acetabular cup and the femoral stem, (p = 0.31 and p = 0.15, respectively).
Conclusions
Our study found no difference between the King Mark method and the conventional metal ball method in the ability to accurately predict component sizes. In the subgroup of obese patients, the King Mark technique offered no advantage for accurately predicting component sizes.



Similar content being viewed by others
References
Shin JK, Son SM, Kim TW et al (2016) Accuracy and reliability of preoperative on-screen templating using digital radiographs for total hip arthroplasty. Hip pelvis 28:201–207. https://doi.org/10.5371/hp.2016.28.4.201
Kosashvili Y, Shasha N, Olschewski E et al (2009) Digital versus conventional templating techniques in preoperative planning for total hip arthroplasty. Can J Surg 52:6–11
Eggli S, Pisan M, Muller ME (1998) The value of preoperative planning for total hip arthroplasty. J Bone Joint Surg Br 80:382–390. https://doi.org/10.1302/0301-620x.80b3.7764
Boese CK, Wilhelm S, Haneder S et al (2019) Influence of calibration on digital templating of hip arthroplasty. Int Orthop 43:1799–1805. https://doi.org/10.1007/s00264-018-4120-7
Alnahhal A, Aslam-pervez N, Sheikh HQ (2019) Templating. Hip Arthroplasty 7:672–685
Baxter JA, Barlow T, Karthikeyan S et al (2012) The accuracy of automatic calibration of digital pelvic radiographs using two different scale markers: a comparative study. Hip Int 22:82–89. https://doi.org/10.5301/HIP.2012.9044
King RJ, Makrides P, Gill JA et al (2009) A novel method of accurately calculating the radiological magnification of the hip. J Bone Joint Surg Br 91:1217–1222. https://doi.org/10.1302/0301-620X.91B9.22615
Franken M, Grimm B, Heyligers I (2010) A comparison of four systems for calibration when templating for total hip replacement with digital radiography. J Bone Joint Surg Br 92:136–141. https://doi.org/10.1302/0301-620X.92B1.22257
Boese CK, Lechler P, Rose L et al (2015) Calibration markers for digital templating in total hip arthroplasty. PLoS ONE 10:e0128529–e0128529. https://doi.org/10.1371/journal.pone.0128529
Boese CK, Wilhelm S, Haneder S et al (2019) Dual-position calibration markers for total hip arthroplasty: theoretical comparison to fixed calibration and single marker method. Int Orthop 43:589–595. https://doi.org/10.1007/s00264-018-4034-4
Bayne CO, Krosin M, Barber TC (2009) Evaluation of the accuracy and use of x-ray markers in digital templating for total hip arthroplasty. J Arthroplasty 24:407–413. https://doi.org/10.1016/j.arth.2007.11.020
Wimsey S, Pickard R, Shaw G (2006) Accurate scaling of digital radiographs of the pelvis. A prospective trial of two methods. J Bone Joint Surg Br 88:1508–1512. https://doi.org/10.1302/0301-620X.88B11.18017
The B, Kootstra JWJ, Hosman AH et al (2007) Comparison of techniques for correction of magnification of pelvic X-rays for hip surgery planning. J Digit Imaging 20:329–335. https://doi.org/10.1007/s10278-006-1042-5
Sershon RA, Diaz A, Bohl DD, Levine BR (2017) Effect of body mass index on digital templating for total hip arthroplasty. J Arthroplasty 32:1024–1026. https://doi.org/10.1016/j.arth.2016.09.020
Kniesel B, Konstantinidis L, Hirschmuller A et al (2014) Digital templating in total knee and hip replacement: an analysis of planning accuracy. Int Orthop 38:733–739. https://doi.org/10.1007/s00264-013-2157-1
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Warschawski, Y., Shichman, I., Morgan, S. et al. The accuracy of external calibration markers in digital templating using the double marker and single marker method: a comparative study. Arch Orthop Trauma Surg 140, 1559–1565 (2020). https://doi.org/10.1007/s00402-020-03569-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03569-2