Abstract
Introduction
The contribution of the glenohumeral joint to shoulder abduction is acknowledged as an important factor for reverse total shoulder arthroplasty (RTSA) patients. In contrast, the degree of scapulothoracic joint contribution and its relation to RTSA patients with poor to excellent shoulder abduction are unclear.
Materials and methods
Twenty-three selectively recruited patients (74 ± 7 years, 11 males) with shoulder abduction ranging from poor to excellent at least 6 months after primary, unilateral RTSA participated in this study. Individual scapulothoracic and glenohumeral contributions at maximum shoulder abduction in the scapular plane were measured using 3D motion capture and correlations between scapulothoracic and glenohumeral contributions to shoulder abduction were assessed. Multiple regression analysis was used to determine the influence of age, body mass index, follow-up period, abduction strength and passive glenohumeral mobility on scapulothoracic and glenohumeral function.
Results
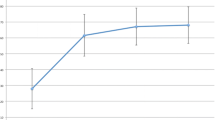
Maximum shoulder abduction (range 48°–140°) was not significantly correlated with the scapulothoracic contribution (range 39°–75°, r = 0.40, p = 0.06), but there was a strong and significant correlation with the glenohumeral contribution (range − 9°–83°, r = 0.91, p < 0.001). Abduction strength was strongly associated with glenohumeral (p = 0.006) but not scapulothoracic (p = 0.34) joint contributions.
Conclusions
Limited shoulder abduction is not associated with insufficient scapulothoracic mobility, which rather provides a basic level of function for RTSA patients. Good to excellent shoulder abduction could only be achieved by increasing the glenohumeral contribution that was associated with postoperative abduction strength.

Similar content being viewed by others

References
Boileau P, Watkinson DJ, Hatzidakis AM, Balg F (2005) Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg 14(1S):147S–161S. https://doi.org/10.1016/j.jse.2004.10.006
Grammont PM, Baulot E (1993) Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 16(1):65–68. https://doi.org/10.3928/0147-7447-19930101-11
Bergmann JH, de Leeuw M, Janssen TW, Veeger DH, Willems WJ (2008) Contribution of the reverse endoprosthesis to glenohumeral kinematics. Clin Orthop Relat Res 466(3):594–598. https://doi.org/10.1007/s11999-007-0091-5
Flurin PH, Marczuk Y, Janout M, Wright TW, Zuckerman J, Roche CP (2013) Comparison of outcomes using anatomic and reverse total shoulder arthroplasty. Bull Hosp Jt Dis 71(Suppl 2):101–107
Lee KW, Kim YI, Kim HY, Yang DS, Lee GS, Choy WS (2016) Three-dimensional scapular kinematics in patients with reverse total shoulder arthroplasty during arm motion. Clin Orthop Surg 8(3):316–324. https://doi.org/10.4055/cios.2016.8.3.316
Werner CM, Steinmann PA, Gilbart M, Gerber C (2005) Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Jt Surg 87(7):1476–1486. https://doi.org/10.2106/JBJS.D.02342
de Toledo JM, Loss JF, Janssen TW, van der Scheer JW, Alta TD, Willems WJ, Veeger DH (2012) Kinematic evaluation of patients with total and reverse shoulder arthroplasty during rehabilitation exercises with different loads. Clin Biomech 27(8):793–800. https://doi.org/10.1016/j.clinbiomech.2012.04.009
Walker D, Matsuki K, Struk AM, Wright TW, Banks SA (2015) Scapulohumeral rhythm in shoulders with reverse shoulder arthroplasty. J Shoulder Elbow Surg 24(7):1129–1134. https://doi.org/10.1016/j.jse.2014.11.043
Kwon YW, Pinto VJ, Yoon J, Frankle MA, Dunning PE, Sheikhzadeh A (2012) Kinematic analysis of dynamic shoulder motion in patients with reverse total shoulder arthroplasty. J Shoulder Elbow Surg 21(9):1184–1190. https://doi.org/10.1016/j.jse.2011.07.031
Roren A, Nguyen C, Palazzo C, Fayad F, Revel M, Gregory T, Poiraudeau S, Roby-Brami A, Lefevre-Colau MM (2017) Kinematic analysis of the shoulder complex after anatomic and reverse total shoulder arthroplasty: a cross-sectional study. Musculoskelet Sci Pract 29:84–90. https://doi.org/10.1016/j.msksp.2017.03.006
Rettig O, Fradet L, Kasten P, Raiss P, Wolf SI (2009) A new kinematic model of the upper extremity based on functional joint parameter determination for shoulder and elbow. Gait Posture 30(4):469–476. https://doi.org/10.1016/j.gaitpost.2009.07.111
Lempereur M, Brochard S, Leboeuf F, Remy-Neris O (2014) Validity and reliability of 3D marker based scapular motion analysis: a systematic review. J Biomech 47(10):2219–2230. https://doi.org/10.1016/j.jbiomech.2014.04.028
Angst F, Goldhahn J, Pap G, Mannion AF, Roach KE, Siebertz D, Drerup S, Schwyzer HK, Simmen BR (2007) Cross-cultural adaptation, reliability and validity of the German Shoulder Pain and Disability Index (SPADI). Rheumatology (Oxford) 46(1):87–92. https://doi.org/10.1093/rheumatology/kel040
Evans JD (1996) Straightforward statistics for the behavioral sciences. Thomson Brooks/Cole Publishing Co, Boston
de Groot JH, Valstar ER, Arwert HJ (1998) Velocity effects on the scapulo-humeral rhythm. Clin Biomech 13(8):593–602. https://doi.org/10.1016/S0268-0033(98)00037-0
Fayad F, Hoffmann G, Hanneton S, Yazbeck C, Lefevre-Colau MM, Poiraudeau S, Revel M, Roby-Brami A (2006) 3-D scapular kinematics during arm elevation: effect of motion velocity. Clin Biomech 21(9):932–941. https://doi.org/10.1016/j.clinbiomech.2006.04.015
Wiater BP, Koueiter DM, Maerz T, Moravek JE Jr, Yonan S, Marcantonio DR, Wiater JM (2015) Preoperative deltoid size and fatty infiltration of the deltoid and rotator cuff correlate to outcomes after reverse total shoulder arthroplasty. Clin Orthop Relat Res 473(2):663–673. https://doi.org/10.1007/s11999-014-4047-2
Yoon JP, Seo A, Kim JJ, Lee CH, Baek SH, Kim SY, Jeong ET, Oh KS, Chung SW (2017) Deltoid muscle volume affects clinical outcome of reverse total shoulder arthroplasty in patients with cuff tear arthropathy or irreparable cuff tears. PLoS ONE 12(3):e0174361. https://doi.org/10.1371/journal.pone.0174361
Jobin CM, Brown GD, Bahu MJ, Gardner TR, Bigliani LU, Levine WN, Ahmad CS (2012) Reverse total shoulder arthroplasty for cuff tear arthropathy: the clinical effect of deltoid lengthening and center of rotation medialization. J Shoulder Elbow Surg 21(10):1269–1277. https://doi.org/10.1016/j.jse.2011.08.049
de Wilde LF, Audenaert EA, Berghs BM (2004) Shoulder prostheses treating cuff tear arthropathy: a comparative biomechanical study. J Orthop Res 22(6):1222–1230. https://doi.org/10.1016/j.orthres.2004.03.010
Jeon YS, Rhee YG (2018) Factors associated with poor active anterior elevation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 27(5):786–793. https://doi.org/10.1016/j.jse.2017.10.027
Ladermann A, Denard PJ, Boileau P, Farron A, Deransart P, Terrier A, Ston J, Walch G (2015) Effect of humeral stem design on humeral position and range of motion in reverse shoulder arthroplasty. Int Orthop 39(11):2205–2213. https://doi.org/10.1007/s00264-015-2984-3
Ladermann A, Lubbeke A, Melis B, Stern R, Christofilopoulos P, Bacle G, Walch G (2011) Prevalence of neurologic lesions after total shoulder arthroplasty. J Bone Jt Surg 93(14):1288–1293. https://doi.org/10.2106/JBJS.J.00369
Boudreau S, Boudreau ED, Higgins LD, Wilcox RB 3rd (2007) Rehabilitation following reverse total shoulder arthroplasty. J Orthop Sports Phys Ther 37(12):734–743. https://doi.org/10.2519/jospt.2007.2562
Namdari S, Yagnik G, Ebaugh DD, Nagda S, Ramsey ML, Williams GR Jr, Mehta S (2012) Defining functional shoulder range of motion for activities of daily living. J Shoulder Elbow Surg 21(9):1177–1183. https://doi.org/10.1016/j.jse.2011.07.032
Acknowledgements
The authors would like to thank M. Wilhelmi, PhD, for the editing of this manuscript.
Funding
The authors declare no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Friesenbichler, B., Grassi, A., Grobet, C. et al. Is limited shoulder abduction associated with poor scapulothoracic mobility after reverse shoulder arthroplasty?. Arch Orthop Trauma Surg 141, 587–591 (2021). https://doi.org/10.1007/s00402-020-03445-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03445-z