Abstract
Purpose
Osgood–Schlatter disease (OSD) is a traction apophysitis of the tibial tuberosity. Patellar tendinopathy and deep infrapatellar bursitis have recently been shown to contribute to pain in patients with OSD. We compared the effects of dextrose injection and saline injection.
Methods
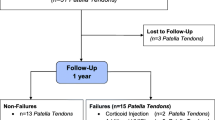
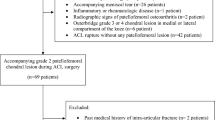
We performed a clinical trial from April 2012 to January 2016 and included 49 knees from 37 boys and 1 girl (mean age, 12.3 ± 1.1 years) for whom conventional conservative therapy for > 1 month was ineffective. They were randomly assigned to receive double-blind injections of 1% lidocaine (1 mL) with 20% dextrose (1 mL; dextrose group) or 1% lidocaine (1 mL) with saline (1 mL; saline group). Injections were administered monthly for 3 months by a single investigator. The Victorian Institute of Sport Assessment (VISA) score was used to evaluate anterior knee pain.
Results
Overall, 43 knees were included; 6 knees were lost to follow-up. The mean pre-injection VISA scores in the dextrose and saline groups were 58.7 ± 18.3 and 63.4 ± 16.4, respectively. No significant differences were found between the two groups at any time point. The mean VISA score before injections significantly increased at the 1-month follow-up in both groups (P < .01). The injection had no adverse effects.
Conclusions
We were not able to show the efficacy of dextrose injections compared to that of saline.
Level of evidence
Randomized controlled trial. Level I.




Similar content being viewed by others
References
Almekinders LC, Temple JD (1998) Etiology, diagnosis, and treatment of tendonitis: an analysis of the literature. Med Sci Sports Exerc 30(8):1183–1190
Banks AR (1991) A rationale for prolotherapy. J Orthop Med 13:54–59
Beyzadeoglu T, Inan M, Bekler H, Altintas F (2008) Arthroscopic excision of an ununited ossicle due to Osgood-Schlatter disease. Arthroscopy 24(9):1081–1083
Czyrny Z (2010) Osgood-Schlatter disease in ultrasound diagnostic–a pictorial essay. Med Ultrason 12(4):323–335
Davis KW (2010) Imaging pediatric sports injuries: lower extremity. Radiol Clin North Am 48(6):1213–1235
ElHusseini TF, Abdelgawad AA (2010) Results of surgical treatment of unresolved Osgood-Schlatter disease in adults. J Knee Surg 23(2):103–107
Gholve PA, Scher DM, Khakharia S, Widmann RF, Green DW (2007) Osgood Schlatter syndrome. Curr Opin Pediatr 19(1):44–50
Hirano A, Fukubayashi T, Ishii T, Ochiai N (2002) Magnetic resonance imaging of Osgood-Schlatter disease: the course of the disease. Skeletal Radiol 31(6):334–342
Jensen KT, Rabago DP, Best TM, Patterson JJ, Vanderby R (2008) Response of knee ligaments to prolotherapy in a rat injury model. Am J Sports Med 36(7):1347–1357
Kader D, Saxena A, Movin T, Maffulli N (2002) Achilles tendinopathy: some aspects of basic science and clinical management. Br J Sports Med 36(4):239–249
Katz JF (1981) Nonarticular osteochondroses. Clin Orthop Relat Res 158:70–76
Kaya DO, Toprak U, Baltaci G, Yosmaoglu B, Ozer H (2013) Long-term functional and sonographic outcomes in Osgood-Schlatter disease. Knee Surg Sports Traumatol Arthrosc 21(5):1131–1139
Khan KM, Cook JL, Maffulli N, Kannus P (2000) Where is the pain coming from in tendinopathy? It may be biochemical, not only structural in origin. Br J Sports Med 34(2):81–83
Krause BL, Williams JP, Catterall A (1990) Natural history of Osgood-Schlatter disease. J Pediatr Orthop 10(1):65–68
Kujala UM, Kvist M, Heinonen O (1985) Osgood-Schlatte’s disease in adolescent athletes. Retrospective study of incidence and duration. Am J Sports Med 13(4):236–241
Maxwell NJ, Ryan MB, Taunton JE, Gillies GH, Wong AD (2007) Sonographically guided intratendinous injection of hyperosmolar dextrose to treat chronic tendinosis of the Achilles tendon: a pilot study. AJR Am J Roentgenol. 189(4):W215–220
McShane JM, Shah VN, Nazarian LN (2008) Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow: is a corticosteroid necessary? J Ultrasound Med 27(8):1137–1144
Mital MA, Matza RA, Cohen J (1980) The so-called unresolved Osgood-Schlatter lesion: a concept based on fifteen surgically treated lesions. J bone Joint Surg Am 62(5):732–739
O’Brien M (1992) Functional anatomy and physiology of tendons. Clin Sports Med 11(3):505–520
Osgood RB (1903) Lesions of the tibial tubercle occurring during adolescence. Boston Med Surg J 148:114–117
Pagenstert G, Wurm M, Gehmert S, Egloff C (2017) Reduction osteotomy of the prominent tibial tubercle after Osgood-Schlatter disease. Arthroscopy 33(8):1551–1557
Ross MD, Villard D (2003) Disability levels of college-aged men with a history of Osgood-Schlatter disease. J Strength Cond Res 17(4):659–663
Ryan M, Wong A, Taunton J (2010) Favorable outcomes after sonographically guided intratendinous injection of hyperosmolar dextrose for chronic insertional and midportion Achilles tendinosis. AJR Am J Roentgenol 194(4):1047–1053
Sanderson LM, Bryant A (2015) Effectiveness and safety of prolotherapy injections for management of lower limb tendinopathy and fasciopathy: a systematic review. J Foot Ankle Res 20(8):57
Schlatter C (1903) Verletzungen der schnabelformigen fortsatzes der obseren tibia epiphyse. Beitr Klin Chir 38:874–887
Topol GA, Reeves KD, Hassanein KM (2005) Efficacy of dextrose prolotherapy in elite male kicking-sport athletes with chronic groin pain. Arch Phys Med Rehabil 86(4):697–702
Topol GA, Podesta LA, Reeves KD, Raya MF, Fukkerton BD, Yeh HW (2010) Hyperosmolar dextrose injection for recalcitrant osgood-schlatter disease. Pediatrics 128(5):e1121–1128
Vreju F, Ciurea P, Rosu A (2010) Osgood-Schlatter disease–ultrasonographic diagnostic. Med Ultrason 12(4):336–339
Wall EJ (1998) Osgood-Schlatter disease: practical treatment for a self-limiting condition. Phys Sportsmed 26(3):29–34
Weiler R (2011) Osgood-Schlatter disease. BMJ 343:d434
Yelland MJ, Sweeting KR, Lyftogt JA, Ng SK, Scuffham PA, Evans KA (2011) Prolotherapy injections and eccentric loading exercises for painful Achilles tendinosis: a randomised trial. Br J Sports Med 45(5):421–428
Author information
Authors and Affiliations
Contributions
JN: prepared the most part of the submitted text (main author) and directed the submitted study, and contributed to the preparation of the Discussion part (corresponding author). TO, YT, KS, and KA: contributed to the discussion on the study design and the preparation of the Materials and methods part. HT: contributed to the discussion on the study design and the preparation of the Discussion part.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakase, J., Oshima, T., Takata, Y. et al. No superiority of dextrose injections over placebo injections for Osgood–Schlatter disease: a prospective randomized double-blind study. Arch Orthop Trauma Surg 140, 197–202 (2020). https://doi.org/10.1007/s00402-019-03297-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03297-2