Abstract
Objective
The objective of the current study was to evaluate the effect of a quality management system on treatment and care delivery of proximal femoral fractures. Specifically, our hypothesis was that the “plan–do–check–act (PDCA)” philosophy of the ISO 9001 quality management system results in a continuous improvement process.
Methods
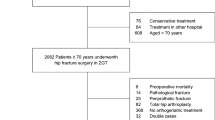
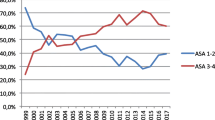
1015 proximal femoral fractures were prospectively included into a hip fracture database over a 5-year period, after a restructuring process with implementation of clinical pathways and standard operation procedures. A close and structured ortho-geriatric co-management (certified ortho-geriatric center) was the basis for treatment. ISO 9001 certification was granted for the first time in 2012. Procedural and patient outcome parameters were analyzed by year and evaluated statistically using SPSS 25.0.
Results
In both categories (procedural and outcome) significant changes could be detected during the 5-year period, e.g., significant reduction of time to surgery for the first 2 years, improvement in discharge management, and reduction of surgical complications. However, no significant changes could be demonstrated for mortality or internal complications such as pneumonia, urinary tract infections, or postoperative delirium. However, the incidence of the latter was already on a very low level at the onset of the quality improvement process.
Conclusion
We could show a relevant and continuous improvement of several quality indicators during a 5-year period after implementation of a quality management system based on the PDCA philosophy for the treatment of proximal femoral fractures in elderly patients. However, other parameters (internal complications, cost-effectiveness, etc.) need our close attention in the future.


Similar content being viewed by others
Notes
Diabetes mellitus with end-organ damage, liver disease, moderate to severe, malignancy, moderate to severe chronic kidney disease, chronic heart failure, myocardial infarction, COPD, dementia, hemiplegia. Corresponding to a Charleston Comorbidity Index of 4 and above and an estimated 10-year survival of less than 50%, the geriatrician responsible decided upon inclusion and exclusion.
Early geriatric rehabilitation program: geriatric and social assessment, weekly teem meeting, activating care of specially trained nursing staff, 20 units of physical and occupational therapy during a 14-day period.
Data not presented.
References
Kanis JA, Johnell O, Oden A, Jonsson B, De Laet C, Dawson A (2000) Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone 27(5):585–590
Veronese N, Maggi S (2018) Epidemiology and social costs of hip fracture. Injury. https://doi.org/10.1016/j.injury.2018.04.015
Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK (2003) The components of excess mortality after hip fracture. Bone 32(5):468–473
Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152(6):380–390. https://doi.org/10.7326/0003-4819-152-6-201003160-00008
Griffin XL, Parsons N, Achten J, Fernandez M, Costa ML (2015) Recovery of health-related quality of life in a United Kingdom hip fracture population. The Warwick Hip Trauma Evaluation—a prospective cohort study. Bone Joint J 97-B(3):372–382. https://doi.org/10.1302/0301-620X.97B3.35738
Cumming RG, Klineberg R, Katelaris A (1996) Cohort study of risk of institutionalisation after hip fracture. Aust N Z J Public Health 20(6):579–582
Leigheb F, Vanhaecht K, Sermeus W, Lodewijckx C, Deneckere S, Boonen S, Boto PA, Mendes RV, Panella M (2012) The effect of care pathways for hip fractures: a systematic review. Calcif Tissue Int 91(1):1–14. https://doi.org/10.1007/s00223-012-9589-2
Vanhaecht K, Sermeus W, Peers J, Lodewijckx C, Deneckere S, Leigheb F, Boonen S, Sermon A, Boto P, Mendes RV, Panella M, EQCP Study Group (2012) The impact of care pathways for patients with proximal femur fracture: rationale and design of a cluster-randomized controlled trial. BMC Health Serv Res 12:124. https://doi.org/10.1186/1472-6963-12-124
Yousefinezhadi T, Mohamadi E, Safari Palangi H, Akbari Sari A (2015) The effect of ISO 9001 and the EFQM model on improving hospital performance: a systematic review. Iran Red Crescent Med J 17(12):e23010. https://doi.org/10.5812/ircmj.23010
Moeller J, Breinlinger-O’Reilly J, Elser J (2000) Quality management in German health care—the EFQM Excellence Model. Int J Health Care Qual Assur Inc Leadersh Health Serv 13(6–7):254–258
Duarte NT, Goodson JR, Arnold EW (2013) Performance management excellence among the Malcolm Baldrige National Quality Award Winners in Health Care. Health Care Manag (Frederick) 32(4):346–358. https://doi.org/10.1097/HCM.0b013e3182a9d704
Tittel S, Burkhardt J, Roll C, Kinner B (2018) Clinical pathways for geriatric patients with proximal femoral fracture improve quality of care delivery and outcome. Orthop Traumatol Surg Res (submitted)
Poksinska B, Dahlgaard JJ, Antoni M (2002) The state of ISO 9000 certification: a study of Swedish organizations. TQM Mag 14(5):297. https://doi.org/10.1108/09544780210439734
Tague NR (2005) “Plan–Do–Study–Act cycle”. The quality toolbox, 2nd edn. ASQ Quality Press, Milwaukee
Logters T, Hakimi M, Linhart W, Kaiser T, Briem D, Rueger J, Windolf J (2008) Early interdisciplinary geriatric rehabilitation after hip fracture: effective concept or just transfer of costs?. Unfallchirurg 111(9):719–726. https://doi.org/10.1007/s00113-008-1469-x
Vogel P, Vassilev G, Kruse B, Cankaya Y (2011) Morbidity and mortality conference as part of PDCA cycle to decrease anastomotic failure in colorectal surgery. Langenbecks Arch Surg 396(7):1009–1015. https://doi.org/10.1007/s00423-011-0820-9
Casaletto JA, Gatt R (2004) Post-operative mortality related to waiting time for hip fracture surgery. Injury 35(2):114–120
Pincus D, Ravi B, Wasserstein D, Huang A, Paterson JM, Nathens AB, Kreder HJ, Jenkinson RJ, Wodchis WP (2017) Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA 318(20):1994–2003. https://doi.org/10.1001/jama.2017.17606
Gulati V, Newman S, Porter KJ, Franco LCS, Wainwright T, Ugoigwe C, Middleton R (2018) Implications of anticoagulant and antiplatelet therapy in patients presenting with hip fractures: a current concepts review. Hip Int 28(3):227–233. https://doi.org/10.1177/1120700018759300
Bohm E, Loucks L, Wittmeier K, Lix LM, Oppenheimer L (2015) Reduced time to surgery improves mortality and length of stay following hip fracture: results from an intervention study in a Canadian health authority. Can J Surg 58(4):257–263
Saez Lopez P, Sanchez Hernandez N, Paniagua Tejo S, Valverde Garcia JA, Montero Diaz M, Alonso Garcia N, Freites Esteve A (2015) Clinical pathway for hip fracture patients. Rev Esp Geriatr Gerontol 50(4):161–167. https://doi.org/10.1016/j.regg.2014.11.003
Sanchez-Hernandez N, Saez-Lopez P, Paniagua-Tejo S, Valverde-Garcia JA (2016) Results following the implementation of a clinical pathway in the process of care to elderly patients with osteoporotic hip fracture in a second level hospital. Rev Esp Cir Ortop Traumatol 60(1):1–11. https://doi.org/10.1016/j.recot.2015.08.001
Lau TW, Leung F, Siu D, Wong G, Luk KD (2010) Geriatric hip fracture clinical pathway: the Hong Kong experience. Osteoporos Int 21(Suppl 4):S627–S636. https://doi.org/10.1007/s00198-010-1387-y
Kalmet PH, Koc BB, Hemmes B, Ten Broeke RH, Dekkers G, Hustinx P, Schotanus MG, Tilman P, Janzing HM, Verkeyn JM, Brink PR, Poeze M (2016) Effectiveness of a multidisciplinary clinical pathway for elderly patients with hip fracture: a multicenter comparative cohort study. Geriatr Orthop Surg Rehabil 7(2):81–85. https://doi.org/10.1177/2151458516645633
Burgers PT, Van Lieshout EM, Verhelst J, Dawson I, de Rijcke PA (2014) Implementing a clinical pathway for hip fractures; effects on hospital length of stay and complication rates in five hundred and twenty six patients. Int Orthop 38(5):1045–1050. https://doi.org/10.1007/s00264-013-2218-5
Flikweert ER, Izaks GJ, Knobben BA, Stevens M, Wendt K (2014) The development of a comprehensive multidisciplinary care pathway for patients with a hip fracture: design and results of a clinical trial. BMC Musculoskelet Disord 15:188. https://doi.org/10.1186/1471-2474-15-188
Koval KJ, Chen AL, Aharonoff GB, Egol KA, Zuckerman JD (2004) Clinical pathway for hip fractures in the elderly: the Hospital for Joint Diseases experience. Clin Orthop Relat Res (425):72–81
Koval KJ, Cooley MR (2005) Clinical pathway after hip fracture. Disabil Rehabil 27(18–19):1053–1060. https://doi.org/10.1080/09638280500056618
Soong C, Cram P, Chezar K, Tajammal F, Exconde K, Matelski J, Sinha SK, Abrams HB, Fan-Lun C, Fabbruzzo-Cota C, Backstein D, Bell CM (2016) Impact of an integrated hip fracture inpatient program on length of stay and costs. J Orthop Trauma 30(12):647–652. https://doi.org/10.1097/BOT.0000000000000691
Becker C (2017) https://www.gesundheitsforschung-bmbf.de/de/PROFinD-2-Osteoporotische-Frakturen-Praevention-und-Rehabilitation.php
Forni S, Pieralli F, Sergi A, Lorini C, Bonaccorsi G, Vannucci A (2016) Mortality after hip fracture in the elderly: the role of a multidisciplinary approach and time to surgery in a retrospective observational study on 23,973 patients. Arch Gerontol Geriatr 66:13–17. https://doi.org/10.1016/j.archger.2016.04.014
Beaupre LA, Cinats JG, Senthilselvan A, Lier D, Jones CA, Scharfenberger A, Johnston DW, Saunders LD (2006) Reduced morbidity for elderly patients with a hip fracture after implementation of a perioperative evidence-based clinical pathway. Qual Saf Health Care 15(5):375–379. https://doi.org/10.1136/qshc.2005.017095
Frolich F, Chmielnicki M, Prokop A (2015) Geriatric complex treatment of proximal femoral fractures? Who profits the most?. Unfallchirurg 118(10):858–866. https://doi.org/10.1007/s00113-013-2554-3
Prokop A, Reinauer KM, Chmielnicki M (2015) Is there sense in having a certified centre for geriatric trauma surgery?. Z Orthop Unfall 153(3):306–311. https://doi.org/10.1055/s-0035-1545710
Marcantonio AJ, Pace M, Brabeck D, Nault KM, Trzaskos A, Anderson R (2017) Team approach: management of postoperative delirium in the elderly patient with femoral-neck fracture. JBJS Rev 5(10):e8. https://doi.org/10.2106/JBJS.RVW.17.00026
Todd KS, Barry J, Hoppough S, McConnell E (2015) Delirium detection and improved delirium management in older patients hospitalized for hip fracture. Int J Orthop Trauma Nurs 19(4):214–221. https://doi.org/10.1016/j.ijotn.2015.03.005
Jost SG, Bonnell M, Chacko SJ, Parkinson DL (2010) Integrated primary nursing: a care delivery model for the 21st-century knowledge worker. Nurs Admin Q 34(3):208–216. https://doi.org/10.1097/NAQ.0b013e3181e7032c
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval by the internal review board (IRB) was obtained.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Roll, C., Tittel, S., Schäfer, M. et al. Continuous improvement process: ortho-geriatric co-management of proximal femoral fractures. Arch Orthop Trauma Surg 139, 347–354 (2019). https://doi.org/10.1007/s00402-018-3086-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3086-7