Abstract
Introduction
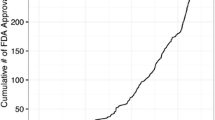
The wide use of hip and knee arthroplasty has led to implementation of volume standards for hospitals and surgeons. For shoulder arthroplasty, the effect of volume on outcome has been researched, but no volume standard exists. This review assessed literature reporting on shoulder arthroplasty volumes and its relation to patient-reported and functional outcomes to define an annual volume threshold.
Materials and methods
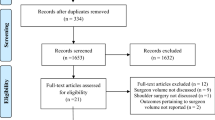
MEDLINE and EMBASE were searched for articles published until February 2018 reporting on the outcome of primary shoulder arthroplasty in relation to surgeon or hospital volume. The primary outcome was predefined as any patient-reported outcome. The secondary outcome measures were length of stay, costs, rates of mortality, complications, readmissions, and revisions. A meta-analysis was performed for outcomes reported by two or more studies.
Results
Eight retrospective studies were included and did not consistently show any associations of volume with in-hospital complications, revision, discharge to home or cost. Volume was consistently associated with length of stay (shorter length of stay for higher volume) and in-hospital complications (fewer in-hospital complications for higher volume). It was not consistently associated with mortality. Functional outcomes were not reported.
Conclusions
There is insufficient evidence to support the concept that only the number of shoulder arthroplasties annually performed (either per hospital or per surgeon) results in better patient-reported and functional outcomes. Currently, published volume thresholds are only based on short-term parameters such as length and cost of hospital stay.







Similar content being viewed by others
References
Zmistowski B, Padegimas EM, Howley M, Abboud J, Williams G Jr, Namdari S (2018) Trends and variability in the use of total shoulder arthroplasty for medicare patients. J Am Acad Orthop Surg 26:133–141. https://doi.org/10.5435/JAAOS-D-16-00720
Hervey SL, Purves HR, Guller U, Toth AP, Vail TP, Pietrobon R (2003) Provider volume of total knee arthroplasties and patient outcomes in the HCUP-nationwide inpatient sample. J Bone Joint Surg Am 85:1775–1783
Ohmann C, Verde PE, Blum K, Fischer B, de Cruppé W, Geraedts M (2010) Two short-term outcomes after instituting a national regulation regarding minimum procedural volumes for total knee replacement. J Bone Joint Surg Am 92:629–638. https://doi.org/10.2106/JBJS.H.01436
Ramkumar PN, Navarro SM, Frankel WC, Haeberle HS, Delanois RE, Mont MA (2018)Evidence-based thresholds for the volume and length of stay relationship in total hip arthroplasty: outcomes and economies of scale. J Arthroplasty. https://doi.org/10.1016/j.arth.2018.01.059 (in press)
Ravi B, Jenkinson R, Austin PC, Croxford R, Wasserstein D, Escott B, Paterson JM, Kreder H, Hawker GA (2014) Relation between surgeon volume and risk of complications after total hip arthroplasty: propensity score matched cohort study. BMJ 23:348
Wilson S, Marx RG, Pan TJ, Lyman S (2016) Meaningful thresholds for the volume-outcome relationship in total knee arthroplasty. J Bone Joint Surg Am 98:1683–1690. https://doi.org/10.2106/JBJS.15.01365
Weinheimer KT, Smuin DM, Dhawan A (2017) Patient outcomes as a function of shoulder surgeon volume: a systematic review. Arthroscopy 33:1273–81. https://doi.org/10.1016/j.arthro.2017.03.005
NICE (National Institute for health and Care Excellence). Guideline scope. Hip, knee and shoulder joint replacement. https://www.nice.org.uk/guidance/gid-ng10084/documents/draft-scope. Accessed 28 Feb 2018
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. https://doi.org/10.1186/2046-4053-4-1
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2011) The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa, ON: Ottawa Hospital Research Institute. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 28 Feb 2018
Hartling L, Milne A, Hamm MP, Vandermeer B, Ansari M, Tsertsvadze A, Dryden DM. Epidemiol (2013) Testing the Newcastle Ottawa Scale showed low reliability between individual reviewers. J Clin 66:982–993. https://doi.org/10.1016/j.jclinepi.2013.03.003
Oremus M, Oremus C, Hall GB, McKinnon MC, ECT & Cognition Systematic Review Team (2012) Inter-rater and test-retest reliability of quality assessments by novice student raters using the Jadad and Newcastle–Ottawa Scales. BMJ open 2:pii:e001368. https://doi.org/10.1136/bmjopen-2012-001368
Singh JA, Ramachandran R (2015) Does hospital volume predict outcomes and complications after total shoulder arthroplasty in the US? Arthritis Care Res (Hoboken) 67:885–890. https://doi.org/10.1002/acr.22507
Day JS, Paxton ES, Lau E, Gordon VA, Abboud JA, Williams GR (2015) Use of reverse total shoulder arthroplasty in the Medicare population. J Shoulder Elbow Surg 24:766–772. https://doi.org/10.1016/j.jse.2014.12.023
Hammond JW, Queale WS, Kim TK, McFarland EG (2003) Surgeon experience and clinical and economic outcomes for shoulder arthroplasty. J Bone Joint Surg Am 85-A:2318–2324
Lyman S, Jones EC, Bach PB, Peterson MG, Marx RG (2005) The association between hospital volume and total shoulder arthroplasty outcomes. Clin Orthop Relat Res 432:132–137
Jain N, Pietrobon R, Hocker S, Guller U, Shankar A, Higgins LD (2004) The relationship between surgeon and hospital volume and outcomes for shoulder arthroplasty. J Bone Joint Surg Am 86:496–505
Jain NB, Kuye I, Higgins LD, Warner JJ (2013) Surgeon volume is associated with cost and variation in surgical treatment of proximal humeral fractures. Clin Orthop Relat Res 47:655–664. https://doi.org/10.1007/s11999-012-2481-6
Ramkumar PN, Navarro SM, Haeberle HS, Ricchetti ET, Iannotti JP (2017) Evidence-based thresholds for the volume-value relationship in shoulder arthroplasty: outcomes and economies of scale. J Shoulder Elbow Surg 26:1399–1406. https://doi.org/10.1016/j.jse.2017.05.019
Singh A, Yian EH, Dillon MT, Takayanagi M, Burke MF, Navarro RA (2014) The effect of surgeon and hospital volume on shoulder arthroplasty perioperative quality metrics. J Shoulder Elbow Surg 23:1187–1194. https://doi.org/10.1016/j.jse.2013.11.017
Amato L, Fusco D, Acampora A, Bontempi K, Rosa AC, Colais P, Cruciani F, D’Ovidio M, Mataloni F, Minozzi S, Mitrova Z, Pinnarelli L, Saulle R, Soldati S, Sorge C, Vecchi S, Ventura M, Davoli M (2017) Volume and health outcomes: evidence from systematic reviews and from evaluation of Italian hospital data. Epidemiol Prev 41(5–6(Suppl 2):1–128. https://doi.org/10.19191/EP17.5-6S2.P001.100
Lau RL, Perruccio AV, Gandhi R, Mahomed NN (2012) The role of surgeon volume on patient outcome in total knee arthroplasty: a systematic review of the literature. BMC Musculoskelet Diso. https://doi.org/10.1186/1471-2474-13-250
Walch G, Bacle G, Lädermann A, Nové-Josserand L, Smithers CJ (2012) Do the indications, results, and complications of reverse shoulder arthroplasty change with surgeon’s experience? J Shoulder Elbow Surg 21:1470–1477. https://doi.org/10.1016/j.jse.2011.11.010
Chowdhury MM, Dagash H, Pierro A (2007) A systematic review of the impact of volume of surgery and specialization on patient outcome. Br J Surg 94:145–161. https://doi.org/10.1002/bjs.5714
Wei DH, Hawker GA, Jevsevar DS, Bozic KJ (2015) Improving value in musculoskeletal care delivery: AOA critical issues. J Bone Joint Surg Am 97:769–774. https://doi.org/10.2106/JBJS.N.00841
Warner JJP, Higgins LD (2017) Editorial commentary: volume and outcome: 100 years of perspective on value From E.A. Codman to M.E. Porter. Arthroscopy 33:1282–1285. https://doi.org/10.1016/j.arthro.2017.03.023
Rasmussen JV, Jakobsen J, Brorson S, Olsen BS (2012) The Danish Shoulder Arthroplasty Registry: clinical outcome and short-term survival of 2,137 primary shoulder replacements. Acta Orthop 83:171–173. https://doi.org/10.3109/17453674.2012.665327
Aveledo R, Holland P, Thomas M, Ashton F, Rangan A (2018) A comparison of the minimum data sets for primary shoulder arthroplasty between national shoulder arthroplasty registries. Is international harmonization feasible? Shoulder Elbow. https://doi.org/10.1177/1758573218755569 (in press)
Acknowledgements
The authors would like to thank Marieke Priester-Vink for assisting with the literature search.
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Kooistra, dr. Flipsen, dr. van den Bekerom, dr. van Raaij, dr. Gosens and dr. van Deurzen declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Kooistra, B.W., Flipsen, M., van den Bekerom, M.P.J. et al. Shoulder arthroplasty volume standards: the more the better?. Arch Orthop Trauma Surg 139, 15–23 (2019). https://doi.org/10.1007/s00402-018-3033-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3033-7