Abstract
Introduction
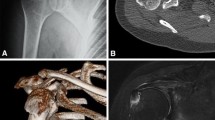
Isolated greater tuberosity (GT) fractures (AO 11-A1) tend to occur in the younger patient population and are poorly managed by most precontoured proximal humerus locking plates. The goal of this study was to identify and assess an alternative treatment strategy for greater tuberosity fractures.
Materials and methods
A retrospective review of all cases of isolated greater tuberosity fractures treated with a 2.4/2.7 mesh plate (Synthes) between 2010 and 2015 was conducted. Patient demographics, operative reports, and clinical notes were reviewed. The time to radiographic union was assessed. Clinical outcomes were retrieved from patients at their follow-up visits or via mailed Disabilities of the Arm, Shoulder, Hand (DASH) questionnaires.
Results
Ten patients with isolated GT fractures treated with mesh plating were identified with an average age of 47.1 years. The average radiographic follow-up was 7.2 months and the average clinical follow-up was 8.0 months. The mean time to union was 8.5 weeks. Two patients underwent elective hardware removal. The mean DASH at final follow-up was 28.2 (±22.4), while the mean DASH work was 13.6 (±19.1).
Conclusion
We have identified a viable alternative treatment option for the surgical management of isolated greater tuberosity fractures using a mesh plate that can be contoured to the patient’s anatomy. Surgeons should be aware of this option for select patients.


Similar content being viewed by others
References
Green A, Izzi J Jr (2003) Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg 12(6):641–649
Court-Brown CM, Garg A, McQueen MM (2001) The epidemiology of proximal humeral fractures. Acta Orthop Scand 72(4):365–371
Gruson KI, Ruchelsman DE, Tejwani NC (2008) Isolated tuberosity fractures of the proximal humeral: current concepts. Injury 39(3):284–298
Park TS, Choi IY, Kim YH, Park MR, Shon JH, Kim SI (1997) A new suggestion for the treatment of minimally displaced fractures of the greater tuberosity of the proximal humerus. Bull Hosp Jt Dis 56(3):171–176
Liao W, Zhang H, Li Z, Li J (2016) Is arthroscopic technique superior to open reduction internal fixation in the treatment of isolated displaced greater tuberosity fractures? Clin Orthop Relat Res 474:1269–1279
Rouleau DM, Mutch J, Laflamme GY (2016) Surgical treatment of displaced greater tuberosity fractures of the humerus. J Am Acad Orthop Surg 24(1):46–56
Platzer P, Thalhammer G, Oberleitner G et al (2008) Displaced fractures of the greater tuberosity: a comparison of operative and nonoperative treatment. J Trauma 65(4):843–848
Sudkamp N, Bayer J, Hepp P et al (2009) Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. results of a prospective, multicenter, observational study. J Bone Joint Surg Am 91(6):1320–1328
Gardner MJ, Griffith MH, Dines JS, Briggs SM, Weiland AJ, Lorich DG (2005) The extended anterolateral acromial approach allows minimally invasive access to the proximal humerus. Clin Orthop Relat Res 434:123–129
Lorich DG, Warner SJ, Schottel PC, Shaffer AD, Lazaro LE, Helfet DL (2015) Multiplanar fixation for patella fractures using a low-profile mesh plate. J Orthop Trauma 29(12):e504–e510
Clavert P, Adam P, Bevort A, Bonnomet F, Kempf JF (2010) Pitfalls and complications with locking plate for proximal humerus fracture. J Shoulder Elbow Surg 19(4):489–494
Schöffl V, Popp D, Strecker W (2011) A simple and effective implant for displaced fractures of the greater tuberosity: the “Bamberg” plate. Arch Orthop Trauma Surg 131(4):509–512
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
The study contains data gathered from the charts of human participants and was approved by the institution’s IRB.
Rights and permissions
About this article
Cite this article
Bogdan, Y., Gausden, E.B., Zbeda, R. et al. An alternative technique for greater tuberosity fractures: use of the mesh plate. Arch Orthop Trauma Surg 137, 1067–1070 (2017). https://doi.org/10.1007/s00402-017-2715-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2715-x