Abstract
Objective
In Achilles tendon injuries, it is suggested that a pathological continuum might be evident from the healthy Achilles tendon to Achilles tendinopathy to Achilles tendon rupture. As such, risk factors for both tendinopathy and rupture should be the same.
Hypothesis
Hereditary and medical risk factors for Achilles tendinopathy and Achilles tendon rupture are the same to a similar extent in a matched pair analysis.
Design
Matched pair study; level of evidence: 3.
Setting
Recreational sportsmen as well as athletes on national level.
Patients
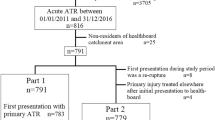
566 questionnaires were analysed. 310 subjects were allocated to 3 groups (A, B, C) after matching the pairs for age, weight, height and gender: (A) healthy Achilles tendons (n = 89, age 39 ± 11 years, BMI 25.1 ± 3.9, females 36%), (B) chronic Achilles tendinopathy (n = 161, age 41 ± 11 years, BMI 24.4 ± 3.7, females 34%), (C) acute Achilles tendon rupture (n = 60, age 40 ± 9 years, BMI 25.2 ± 3.2, females 27%).
Results
We found a positive family history of Achilles tendinopathy as a risk factor for Achilles tendinopathy (OR: 4.8, 95% CI: 1.1–21.4; p = 0.023), but not for Achilles tendon rupture (OR: 4.0, 95% CI 0.7–21.1, p = 0.118). Smoking and cardiac diseases had a lower incidence in Achilles tendinopathy than in healthy subjects (both p = 0.001), while cardiovascular medication did not change the risk profile.
Conclusion
Identifying risk factors associated with Achilles tendon disorders has a high clinical relevance regarding the development and implementation of prevention strategies and programs. This cross-sectional study identified a positive family history as a significant solitary risk factor for Achilles tendinopathy, increasing the risk fivefold. However, in this matched pair analysis excluding age, weight, height and gender as risk factors no further factor necessarily increases the risk for either Achilles tendinopathy or Achilles tendon rupture.
Similar content being viewed by others
References
Knobloch K, Yoon U, Vogt PM (2009) Acute and overuse injuries correlated to hours of training in master running athletes. Foot Ankle Int 29(7):671–676
Sankey RA, Brooks JH, Kemp SP, Haddad FS (2008) The epidemiology of ankle injuries in professional rugby union players. Am J Sports Med 36(12):2415–2424
Parekh SG, Wray WH III, Brimmo O, Sennett BJ, Wapner KL (2009) Epidemiology and outcomes of Achilles tendon ruptures in the National Football League. Foot Ankle Spec. 2(6):283–286 Epub 2009 Oct 13
Tallon C, Maffulli N, Ewen SW (2001) Ruptured Achilles tendons are significantly more degenerated than tendinopathic tendons. Med Sci Sports Exerc 33(12):1983–1990
Van Mechelen W, Hlobil H, Kemper HC (1992) Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Med 14(2):82–99
Gaida JE, Alfredson L, Kiss ZS, Wilson AM, Alfredson H, Cook JL (2009) Dyslipidemia in Achilles tendinopathy is characteristic of insulin resistance. Med Sci Sports Exerc 41(6):1194–1197
Mokone GG, Gajjar M, September AV, Schwellnus MP, Greenberg J, Noakes TD, Collins M (2005) The Guanine-thymine dinucleotide repeat polymorphism within the tenascin-C gene is associated with Achilles tendon injuries. Am J Sports Med 33:1016–1021
Collins M, Posthumus M, Schwellnus MP (2010) The COL1A1 gene and acute soft tissue ruptures. Br J Sports Med 44(14):1063–1064 Epub 2009 Feb 4.PMID: 19193665
Vandenbrouke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M for the STROBE Initiative (2007) Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Ann Intern Med 147(8):W163–W194 PMID:17938389
Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD (2002) A retrospective case–control analysis of 2002 running injuries. Br J Sports Med 36(2):95–101
Longo UG, Rittweger J, Garau G, Radonic B, Gutwasser C, Gilliver SF, Kusy K, Zielinski J, Felsenberg D, Maffulli N (2009) No influence of age, gender, weight, height, and impact profile in Achilles tendinopathy in masters track and field athletes. Am J Sports Med 37(7):1400–1405 Epub 2009 Mar 27. PMID:19329789
Lees JF, Bulleid NJ (1994) The role of cysteine residues in the folding and association of the COOH-terminal propeptide of types I and III procollagen. J Biol Chem 269(39):24354–24360
September AV, Cook J, Handley CJ, van der Merwe L, Schwellnus MP, Collins M (2009) Variants within the COL5A1 gene are associated with Achilles tendinopathy in two populations. Br J Sports Med 43(5):357–365 Epub 2008 Apr 28. PMID:18443036
Beeharry D, Coupe B, Benbow EW, Morgan J, Kwok S, Charlton-Menys V, France M, Durrington PN (2006) Familial hypercholesterolaemia commonly presents with Achilles tenosynovitis. Ann Rheum Dis 65(3):312–315
Smithard A, Lamyman MJ, McCarthy CL, Gibbons CL, Cooke PJ, Athanasou N (2007) Cerebrotendinous xanthomatosis presenting with bilateral Achilles tendon xanthomata. Skeletal Radiol 36(2):171–175 Epub 2006 May 20. PMID:16715243
Holmes GB, Lin J (2006) Etiologic factors associated with symptomatic Achilles tendinopathy. Foot Ankle Int 27(11):952–959
Gaida JE, Alfredson H, Kiss ZS, Bass SL, Cook JL (2010) Asymptomatic Achilles tendon pathology is associated with a central fat distribution in men and aperipheral fat distribution in women: a cross-sectional study of 298 individuals. BMC Musculoskelet Disord 2(11):41
Holmes GB, Mann RAL (1992) Possible epidemiological factors associated with rupture of the posterior tibial tendon. Foot Ankle 13(2):70–79
Sode J, Obel N, Hallas J, Lassen A (2007) Use of fluroquinolone and risk of Achilles tendon rupture: a population-based cohort study. Eur J Clin Pharmacol 63(5):499–503
de Jonge S, van den Berg C, de Vos RJ, van der Heide HJ, Weir A, Verhaar JA, Bierma-Zeinstra SM, Tol JL (2011) Incidence of midportion Achilles tendinopathy in the general population. Br J Sports Med 45(13):1026–1028
Author information
Authors and Affiliations
Corresponding author
Additional information
R. Kraemer and W. Wuerfel contributed equally to this work.
Rights and permissions
About this article
Cite this article
Kraemer, R., Wuerfel, W., Lorenzen, J. et al. Analysis of hereditary and medical risk factors in Achilles tendinopathy and Achilles tendon ruptures: a matched pair analysis. Arch Orthop Trauma Surg 132, 847–853 (2012). https://doi.org/10.1007/s00402-012-1476-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1476-9