Abstract
Background
The most important individual parameter linked to functional outcome following hemiarthroplasty for fractures of the proximal humerus is anatomical healing of the tuberosities. The aim of our study was to evaluate whether the fixation method influences tuberosity healing and functional outcome.
Methods
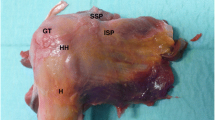
Twenty-five consecutive patients with acute 4-part fractures of the proximal humerus were treated with hemiarthroplasty and cable fixation of the tuberosities. Twenty-nine previous patients with four-part fractures treated with hemiarthroplasty and suture fixation of the tuberosities were included as a control group. Functional evaluation was measured with the Constant Score 1 year after the operation. Radiographic evaluation included evaluation of the extent of tuberosity healing and head centralisation.
Results
The average Constant Score was 53.2 points in the suture group and 60.9 in the cable group (p = 0.29). An x-ray evaluation revealed that 40% of the tuberosities in the suture group were anatomically healed versus 75% (p = 0.027) in the cable group. In the suture group, 44% of the prostheses showed marked superior migration, whereas 25% of the prostheses in the cable group showed such migration (p = 0.027).
Conclusion
In our collective adding an encircling steel cable for the fixation of the tuberosities resulted in higher anatomical healing rates.







Similar content being viewed by others
References
Neer CS 2nd (1970) Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am 52(6):1090–1103
Kralinger F, Schwaiger R, Wambacher M, Farrell E, Menth-Chiari W, Lajtai G, Hubner C, Resch H (2004) Outcome after primary hemiarthroplasty for fracture of the head of the humerus. A retrospective multicentre study of 167 patients. J Bone Joint Surg Br 86(2):217–219. doi:10.1302/0301-620X.86B2.14553
Mighell MA, Kolm GP, Collinge CA, Frankle MA (2003) Outcomes of hemiarthroplasty for fractures of the proximal humerus. J Shoulder Elbow Surg 12(6):569–577. doi:10.1016/S1058274603002131
Robinson CM, Page RS, Hill RM, Sanders DL, Court-Brown CM, Wakefield AE (2003) Primary hemiarthroplasty for treatment of proximal humeral fractures. J Bone Joint Surg Am 85-A(7):1215–1223
Boileau P, Krishnan SG, Tinsi L, Walch G, Coste JS, Mole D (2002) Tuberosity malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg 11(5):401–412. doi:10.1067/mse.2002.124527
Loew M, Heitkemper S, Parsch D, Schneider S, Rickert M (2006) Influence of the design of the prosthesis on the outcome after hemiarthroplasty of the shoulder in displaced fractures of the head of the humerus. J Bone Joint Surg Br 88(3):345–350. doi:10.1302/0301-620X.88B3.16909
Frankle MA, Ondrovic LE, Markee BA, Harris ML, Lee WE 3rd (2002) Stability of tuberosity reattachment in proximal humeral hemiarthroplasty. J Shoulder Elbow Surg 11(5):413–420. doi:10.1067/mse.2002.126098
Krause FG, Huebschle L, Hertel R (2007) Reattachment of the tuberosities with cable wires and bone graft in hemiarthroplasties done for proximal humeral fractures with cable wire and bone graft: 58 patients with a 22-month minimum follow-up. J Orthop Trauma 21(10):682–686. doi:10.1097/BOT.0b013e31815917e0
Neer CS 2nd (1970) Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 52(6):1077–1089
Greiner SH, Diederichs G, Kroning I, Scheibel M, Perka C (2009) Tuberosity position correlates with fatty infiltration of the rotator cuff after hemiarthroplasty for proximal humeral fractures. J Shoulder Elbow Surg 18(3):431–436. doi:10.1016/j.jse.2008.10.007
Konrad GG, Mehlhorn A, Kuhle J, Strohm PC, Sudkamp NP (2008) Proximal humerus fractures—current treatment options. Acta Chir Orthop Traumatol Cech 75(6):413–421
Boileau P, Caligaris-Cordero B, Payeur F, Tinsi L, Argenson C (1999) Prognostic factors during rehabilitation after shoulder prostheses for fracture. Rev Chir Orthop Reparatrice Appar Mot 85(2):106–116
Demirhan M, Akpinar S, Atalar AC, Akman S, Akalin Y (1998) Primary replacement of the humeral head in iatrogenically displaced fracture-dislocations of the shoulder: a report about six cases. Injury 29(7):525–528
Frankle MA, Greenwald DP, Markee BA, Ondrovic LE, Lee WE 3rd (2001) Biomechanical effects of malposition of tuberosity fragments on the humeral prosthetic reconstruction for four-part proximal humerus fractures. J Shoulder Elbow Surg 10(4):321–326. doi:10.1067/mse.2001.113962
Fialka C, Stampfl P, Arbes S, Reuter P, Oberleitner G, Vecsei V (2008) Primary hemiarthroplasty in four-part fractures of the proximal humerus: randomized trial of two different implant systems. J Shoulder Elbow Surg 17(2):210–215. doi:10.1016/j.jse.2007.07.002
Bufquin T, Hersan A, Hubert L, Massin P (2007) Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br 89(4):516–520. doi:10.1302/0301-620X.89B4.18435
Cazeneuve JF, Cristofari DJ (2006) Grammont reversed prosthesis for acute complex fracture of the proximal humerus in an elderly population with 5 to 12 years follow-up. Rev Chir Orthop Reparatrice Appar Mot 92(6):543–548
Wall B, Walch G (2007) Reverse shoulder arthroplasty for the treatment of proximal humeral fractures. Hand Clin 23 (4):425-430, v-vi. doi:10.1016/j.hcl.2007.08.002
Nijs S, Lerut P, Broos P The non-reconstructable proximal humerus fracture: reversed or anatomical arthroplasty? In: Supplement: 7th European Trauma Congress, Ljubljana, 2006. p 222
Hettrich CM, Boraiah S, Dyke JP, Neviaser A, Helfet DL, Lorich DG (2010) Quantitative assessment of the vascularity of the proximal part of the humerus. J Bone Joint Surg Am 92(4):943–948. doi:10.2106/JBJS.H.01144
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dietz, SO., Broos, P. & Nijs, S. Suture fixation versus cable cerclage of the tuberosities in shoulder arthroplasty-clinical and radiologic results. Arch Orthop Trauma Surg 132, 793–800 (2012). https://doi.org/10.1007/s00402-012-1470-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1470-2